Oral Cancer Risk Assessment Tool
This tool estimates your personal oral cancer risk based on key factors. Enter your information to receive tailored prevention recommendations.
Imagine catching a serious disease before it ever takes hold. That’s the promise of Oral cancer prophylaxis-a blend of habits, checks, and interventions designed to keep malignant cells from ever forming in the mouth. In this guide we’ll break down why prevention matters, which actions really work, and how you can build a practical plan that fits everyday life.
Key Takeaways
- Primary risk factors for oral cancer are tobacco, alcohol, and high‑risk HPV.
- Prophylaxis combines lifestyle change, vaccination, chemoprevention, and regular dental screening.
- HPV vaccination before age 26 cuts the risk of HPV‑related oral cancers by up to 90%.
- Daily oral hygiene and biannual dental visits catch precancerous lesions early.
- Evidence‑based chemopreventive agents (e.g., retinoids, green‑tea polyphenols) are useful for high‑risk patients.
What Is Oral Cancer?
Oral Cancer refers to malignant tumors that develop in any part of the mouth-lips, tongue, gums, floor of the mouth, or palate. Globally, more than 350,000 new cases are diagnosed each year, and late‑stage disease carries a five‑year survival rate below 50%. Early detection dramatically improves outcomes, which is why prevention receives so much attention.
Understanding Prophylaxis
Prophylaxis is the set of actions taken to stop disease before it starts. In oral health, prophylaxis includes lifestyle modifications, vaccinations, chemopreventive agents, and routine examinations aimed at lowering the chance that abnormal cells become cancerous. It’s different from treatment-here we’re trying to keep the problem from ever appearing.

Why Risk Factors Matter
Three culprits dominate the oral‑cancer landscape:
- Tobacco use includes smoking cigarettes, cigars, pipes, and smokeless forms such as chewing tobacco. It contributes to roughly 75% of oral cancers.
- Alcohol consumption particularly heavy or chronic drinking, works synergistically with tobacco to raise risk several‑fold.
- Human papillomavirus (HPV) high‑risk strains, especially HPV‑16, are now linked to a growing share of oropharyngeal cancers, even in non‑smokers.
Each factor creates genetic or cellular changes that can evolve into cancer. Effective prophylaxis targets these pathways directly.
Proven Prophylactic Strategies
Below is a quick snapshot of the most evidence‑backed measures.
| Intervention | How It Works | Evidence Level | Typical Recommendation |
|---|---|---|---|
| Tobacco cessation | Removes carcinogens, restores oral mucosa | Strong | Quit completely; use nicotine‑replacement if needed |
| Alcohol moderation | Reduces acetaldehyde exposure | Moderate | Limit to ≤2 drinks/day for men, ≤1 for women |
| HPV vaccination | Prevents infection with high‑risk HPV strains | Strong (90% risk reduction) | Two‑dose series before age 26; consider up to age 45 |
| Dental screening | Early visual detection of leukoplakia, erythroplakia | Strong | Professional exam every 6‑12 months |
| Chemoprevention agents | Inhibit cellular proliferation or promote apoptosis | Emerging | Use in high‑risk patients under clinician supervision |
Lifestyle Modifications
Quitting tobacco is the single most impactful step. Counseling, medications like varenicline, and support groups boost success rates. Cutting alcohol intake further lowers the combined risk. A diet rich in fruits, vegetables, and especially antioxidants (vitamin C, lycopene) offers a modest protective effect.
Oral Hygiene and Dental Check‑ups
Dental check‑up A biannual visit that includes visual inspection of the oral cavity, brush‑up cleaning, and, when needed, adjunctive tools like autofluorescence devices. Maintaining plaque‑free teeth with fluoridated toothpaste reduces chronic inflammation-a known facilitator of malignant transformation.
HPV Vaccination
Vaccination The 9‑valent HPV vaccine protects against high‑risk strains linked to oral and cervical cancers. Studies up to 2024 show a 90% drop in HPV‑related oropharyngeal cancer among vaccinated cohorts. Even adults up to 45years benefit, though the protective gain diminishes with age.
Chemoprevention Agents
Several compounds show promise for people with confirmed oral premalignant lesions:
- Retinoids VitaminA derivatives that normalize epithelial growth; topically applied to oral leukoplakia in controlled trials.
- Green‑tea polyphenol (EGCG) - antioxidant with laboratory evidence of inhibiting tumor cell proliferation.
- COX‑2 inhibitors - reduce inflammatory pathways that can drive cancer, used cautiously due to cardiovascular risks.
These agents aren’t over‑the‑counter solutions; they require prescription and monitoring.
Screening Programs
Regular visual exams remain the backbone of early detection. In high‑risk populations, adjuncts such as oral brush biopsies, toluidine blue staining, or DNA‑based salivary tests improve sensitivity. However, cost and accessibility limit widespread adoption, making basic dental exams the most practical prophylactic tool.
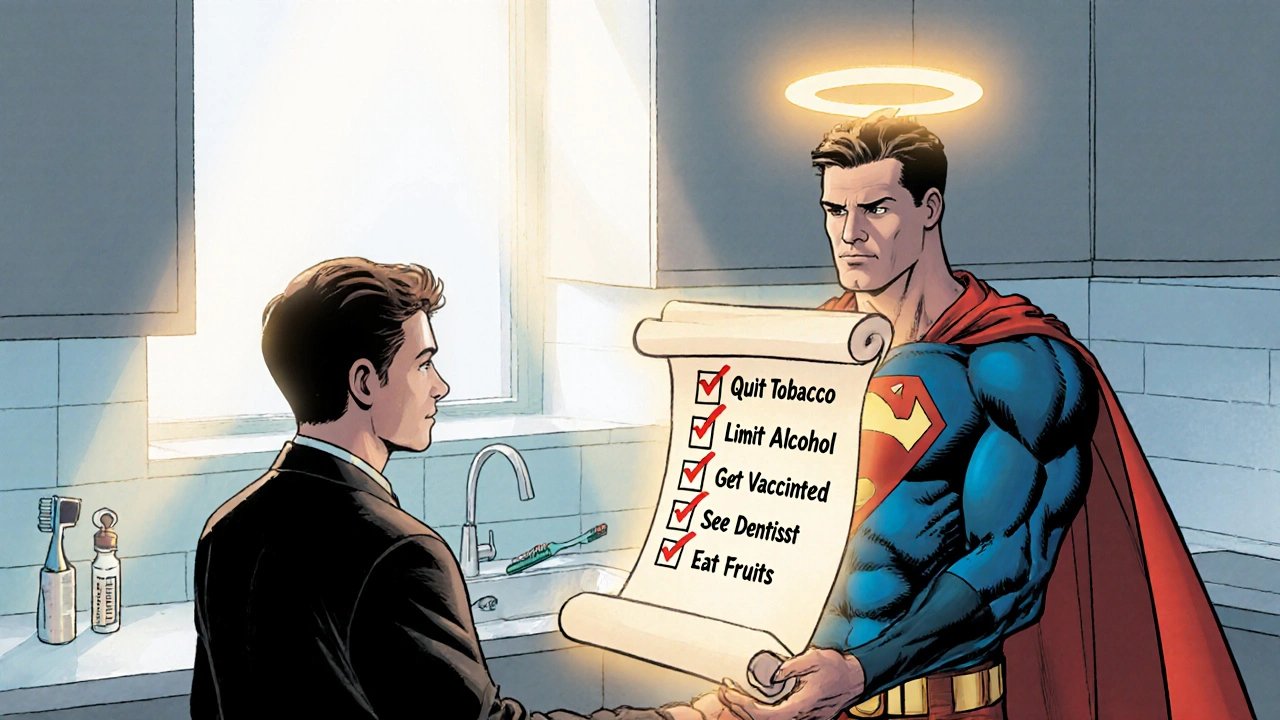
Building Your Personal Prophylaxis Plan
- Assess risk - consider smoking history, alcohol use, and HPV exposure.
- Schedule a dental check‑up if you haven’t had one in the past year.
- Quit tobacco - use counseling, nicotine‑replacement, or prescription meds.
- Limit alcohol - track drinks and set weekly caps.
- Get the HPV vaccine - discuss with your primary‑care provider.
- Adopt a nutrient‑rich diet - aim for at least five servings of fruits/vegetables daily.
- Talk to a specialist about chemoprevention if you have a precancerous lesion.
- Maintain oral hygiene - brush twice daily with fluoridated toothpaste and floss.
Follow this checklist and revisit it every six months. Adjustments are easy once you see the benefits of fewer cravings, fresher breath, and peace of mind.
Common Myths and Pitfalls
Myth: “If I never smoke, I’m safe.” Reality: Alcohol and HPV still pose risks, especially for men over 40. Myth: “A strong mouthwash can replace dental visits.” Reality: Mouthwash may reduce bacteria temporarily but cannot spot early lesions. Pitfall: “Self‑diagnosing a white patch and ignoring it.” A white patch could be harmless, but it could also be early leukoplakia; professional evaluation is essential.
Future Directions
Researchers are honing salivary DNA tests that could flag oncogenic HPV or mutation signatures before any visual sign appears. Meanwhile, vaccine formulations covering even more HPV strains are in phaseIII trials, promising broader protection. For clinicians, integrating risk‑assessment tools into electronic health records will make personalized prophylaxis louder and clearer.
Frequently Asked Questions
Can oral cancer be prevented entirely?
No single strategy guarantees 100% protection, but combining lifestyle change, vaccination, and regular screening reduces risk dramatically-often by 70‑90% for high‑risk groups.
At what age should I get the HPV vaccine for oral cancer prevention?
The ideal window is ages 11‑12, but catch‑up vaccination is recommended up to age 26 and may be considered through age 45 after a risk discussion with a healthcare provider.
How often should I see my dentist for cancer screening?
A professional oral exam every six to twelve months is advised, especially if you have known risk factors like tobacco use or a family history of oral cancer.
Are there over‑the‑counter supplements that help prevent oral cancer?
Evidence for most supplements is limited. Antioxidant‑rich foods are more reliable than pills, and any supplement regimen should be discussed with a clinician.
What signs should prompt an immediate dental visit?
Persistent white or red patches, unexplained lumps, bleeding gums, a sore that won’t heal, or a change in voice or swallowing should all trigger a prompt evaluation.




namrata srivastava
October 16, 2025 at 16:52From an epidemiological stratification standpoint, the prophylactic paradigm delineated herein leverages a confluence of primary and secondary preventive modalities, each underpinned by robust meta‑analytic evidence. The discourse on tobacco cessation, for instance, invokes nicotine‑replacement therapeutics and behavioral contingency frameworks, thereby attenuating the mutagenic burden at the mucosal interface. Concurrently, the inclusion of high‑valent HPV immunization constitutes a serological shield, effecting a quantifiable decrement in oncogenic epitope exposure. While the guide duly appraises chemopreventive agents, it is imperative to contextualize retinoid pharmacodynamics within the broader spectrum of epidermal differentiation pathways. Moreover, the iterative cadence of biannual dental examinations operationalizes a surveillance algorithm that aligns with contemporary risk‑adjusted screening heuristics. In sum, the synthesis of lifestyle, immunologic, and pharmacologic vectors constitutes a multidimensional prophylactic architecture of appreciable clinical merit.
Priyanka arya
October 16, 2025 at 23:48Yo, they don’t want you to know that the “big pharma” push for chemoprevention is just a cash cow 🐄💸. They sprinkle green‑tea polyphenols into every supplement aisle while the real solution-nothing but a clean mouth and a vaccine-gets buried under glossy ads. And those “salivary DNA tests” they hype? Probably a way to collect your genetic data for the next surveillance program 🤖. Stay skeptical, question the hype, and don’t let the gloss sell you a false sense of safety 😤.
Loren Kleinman
October 17, 2025 at 06:45Prophylaxis in oral health is more than a buzzword; it is a disciplined routine that aligns personal habits with scientific evidence. When we consider the major risk factors-tobacco, alcohol, and HPV-we see that each one operates through distinct biological pathways that ultimately converge on DNA damage. Therefore, a successful preventive plan must address each pathway in turn, rather than offering a one‑size‑fits‑all solution. The first pillar, tobacco cessation, removes a constant source of carcinogenic nitrosamines from the oral cavity. Studies have shown that even after years of smoking, the mucosa begins to recover within months of quitting, which reduces the mutation load. The second pillar, moderation of alcohol, lowers the exposure to acetaldehyde, a metabolite that synergizes with tobacco to amplify mutagenic risk. Cutting back to recommended limits not only benefits the liver but also diminishes the oxidative stress in the mouth. The third pillar, HPV vaccination, provides a pre‑emptive immunologic barrier that blocks the entry of high‑risk viral strains into epithelial cells. The data up to 2024 indicate a near‑90 % reduction in HPV‑related oropharyngeal cancers for those vaccinated before the age of 26. Beyond vaccines, regular dental screenings serve as a sentinel system that can catch early leukoplakia or erythroplakia before they progress. A biannual visit that includes visual inspection, adjunctive fluorescence tools, and opportunistic brush biopsies creates a safety net for high‑risk individuals. Complementary to these measures, diet rich in antioxidants-vitamin C, lycopene, and polyphenols-offers a modest but measurable protective effect. While the evidence for over‑the‑counter chemopreventive pills remains inconclusive, prescription‑grade retinoids have demonstrated efficacy in controlled trials for confirmed precancers. It is essential, however, to use such agents under strict medical supervision because of their potential systemic side effects. Putting all these components together into a personal plan requires self‑assessment, goal setting, and periodic review, much like any other health regimen. Ultimately, the convergence of lifestyle modification, immunization, vigilant screening, and targeted pharmacology can shift the odds dramatically in favor of a cancer‑free future.
Sabrina Goethals
October 17, 2025 at 13:42hmm, i guess i never thought about how a simple mouthwash could mask bigger issues. keeping up with the dentist every six months sounds like a good habit, especially if you’ve got a coffee habit that stains your teeth. also, flossing is underrated – it helps keep the gums healthy and might lower inflammation, which is a factor in cancer risk. so yeah, just bite the bullet and book that appointment.
Jenny Spurllock
October 17, 2025 at 20:38Regular visual checks are crucial because many early lesions are asymptomatic, and early intervention can spare patients from extensive treatment later on.
Amanda Joseph
October 18, 2025 at 03:35Great, another checklist to ignore.
Kevin Aniston
October 18, 2025 at 10:32Look, if you’re trying to overhaul your health, start with the low‑hanging fruit: ditch cigarettes, cut back on beer, and schedule that dental exam. Those three steps alone can shift your risk profile dramatically. On top of that, the HPV vaccine isn’t just for teens; adults up to 45 can still reap a huge protective benefit, so talk to your primary care doc about it. When it comes to diet, think rainbow – plenty of berries, leafy greens, and cruciferous veggies that are packed with antioxidants. And if you happen to have a precancerous lesion, don’t panic; discuss chemoprevention options like topical retinoids with an oral medicine specialist. Consistency is key, so set reminders for your appointments and keep a simple log of your habits. Over time you’ll notice better breath, fewer cravings, and the peace of mind that comes from actively guarding your health. It’s a marathon, not a sprint, but each positive habit you lock in is a win for your future self.
Karen Wolsey
October 18, 2025 at 17:28So apparently the secret to not getting oral cancer is “just brush your teeth and get a vaccine,” as if that’s a plug‑and‑play solution for everyone. Sure, good hygiene helps, but let’s not pretend it eliminates the damage done by years of smoking or heavy drinking. The reality is a spectrum of risk, and a one‑sentence punchline doesn’t capture the nuance. Still, if you’re looking for a quick fix, remember there’s no shortcut – the only reliable path is consistent prevention and professional care.
Melissa H.
October 19, 2025 at 00:25Enough with the wishful thinking – the data are crystal clear: tobacco and alcohol are the biggest killers, and the HPV vaccine slashes risk dramatically 😊. If you’re serious about protecting yourself, start cutting the booze, quit smoking, and book that vaccination visit. No more excuses.
Edmond Abdou
October 19, 2025 at 07:22Everyone’s journey to better oral health looks a bit different, but the core steps are universal: quit tobacco, moderate alcohol, stay up-to-date on HPV vaccination, and keep those dental appointments. If you need resources or support, there are community programs and online forums that can help you stay on track 😊. Remember, small consistent actions add up to big protection over time.
Sydnie Baker
October 19, 2025 at 14:18One must underscore the lexical precision inherent in delineating “prophylactic interventions” versus mere “preventive advice.” The former encapsulates empirically validated modalities, each accompanied by statistically significant effect sizes, whereas the latter often devolves into colloquial platitudes. Moreover, the orthographic integrity of terms such as “epithelial dysplasia” and “oncogenic virulence” must be maintained to preserve scholarly rigor.
Benjie Gillam
October 19, 2025 at 21:15Alright, so let’s break down the chemoprevention landscape. Retinoids, especially 13‑cis‑retinoic acid, act on the RA receptor pathway to normalize epithelial turnover – think of it as resetting the growth program. Green‑tea polyphenols (EGCG) inhibit PI3K/Akt signaling, which can curb tumor cell proliferation in vitro. COX‑2 inhibitors, like celecoxib, reduce prostaglandin‑mediated inflammation, but watch out for cardiovascular risk – it’s a trade‑off. All these agents require a prescription and close monitoring because dosing nuances can swing outcomes from beneficial to harmful. So, if you’ve got a confirmed leukoplakia, bring these options to your oral medicine specialist for a tailored plan.
Naresh Sehgal
October 20, 2025 at 04:12Listen up! You’ve got the power to slash your cancer risk, but you’ve got to act NOW. Quit the damn cigarettes, dump the cheap beer, and get that HPV jab before it’s too late. No more whining about “later” – the time for action is today, and if you need a push, hit the gym, join a support group, and hold yourself accountable. This is your health, own it!
Poppy Johnston
October 20, 2025 at 11:08Hey folks, just wanted to say that I started flossing daily and finally booked my dental cleaning after ages – feels awesome! Also, I got the HPV vaccine on a weekend visit, and the staff was super friendly. If anyone’s on the fence, trust me, it’s worth it and makes you feel like you’re actually doing something for yourself.
Johnny VonGriz
October 20, 2025 at 18:05That was a solid rundown, Loren. I’d add that for patients with a family history of oral cancer, genetic counseling can further refine risk stratification. Also, incorporating saliva‑based HPV testing into routine check‑ups could catch silent infections early, though cost remains a barrier. Ultimately, a collaborative approach between dentists, primary care physicians, and oncologists ensures the preventive plan is comprehensive and personalized.
Real Strategy PR
October 21, 2025 at 01:02While skepticism has its place, spreading unfounded claims undermines public health initiatives that have demonstrably reduced cancer incidence.