Venlafaxine Blood Pressure Risk Calculator
How Your Venlafaxine Dose Affects Blood Pressure
Based on clinical studies, venlafaxine can cause a gradual increase in blood pressure, especially at higher doses. This calculator estimates potential blood pressure changes and risk level based on your dose.
When you start taking venlafaxine for depression or anxiety, you’re likely focused on how it will make you feel-less overwhelmed, more like yourself. But there’s one side effect that doesn’t get talked about enough: blood pressure. It’s not rare. It’s not theoretical. And if you’re not watching for it, it can sneak up on you.
Why Venlafaxine Raises Blood Pressure
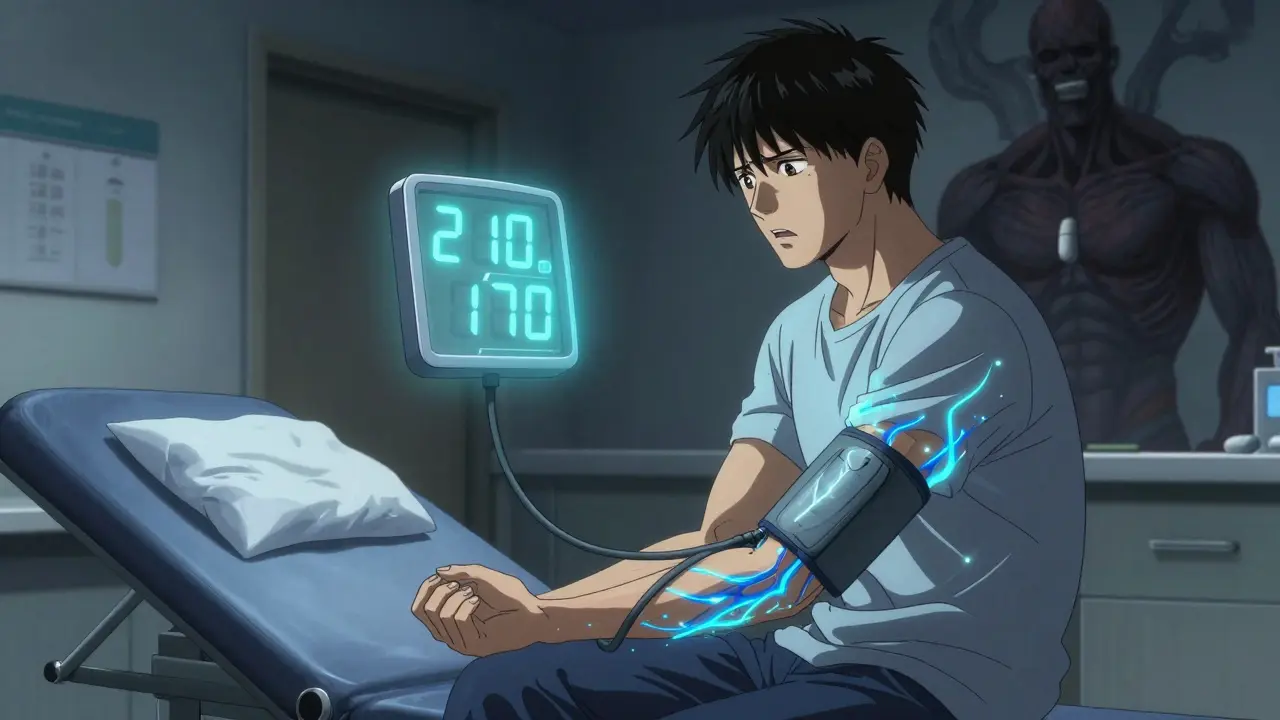
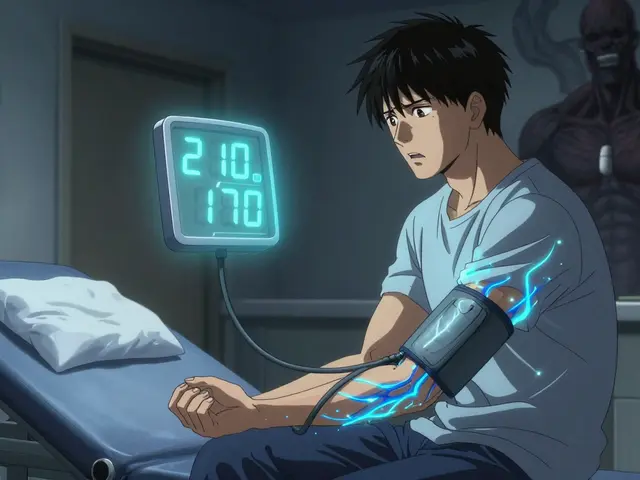
Venlafaxine works differently than most antidepressants. While SSRIs like sertraline or fluoxetine mostly boost serotonin, venlafaxine (sold as Effexor or Effexor XR) also blocks the reuptake of norepinephrine. That’s the key. Norepinephrine is your body’s natural stress hormone. It tightens blood vessels, speeds up your heart, and pushes blood pressure higher. At low doses (under 150 mg/day), the effect is mild. But above that, norepinephrine kicks in hard-and so does the rise in blood pressure. This isn’t just a theory. A major analysis of over 3,700 patients found that venlafaxine caused a small but real increase in diastolic blood pressure-usually 1 to 3 mmHg at standard doses. But when doses go above 300 mg/day, the risk jumps. About 13% of people on high doses developed clinically high blood pressure, compared to just 5% on placebo. And here’s the catch: you don’t need a high dose for this to happen. One case study described a 23-year-old man with no history of high blood pressure. He started venlafaxine at 150 mg/day for depression. Ten months later, his blood pressure hit 210/170 mmHg. That’s a hypertensive crisis-enough to cause stroke or kidney damage. He had no warning signs. No family history. Just venlafaxine and a body that reacted unpredictably.How It Compares to Other Antidepressants
Not all antidepressants affect blood pressure the same way. SSRIs? Rarely. Fluoxetine and sertraline might cause a tiny shift, but nothing that requires monitoring. Tricyclics like amitriptyline? They often cause low blood pressure, especially when standing up. Venlafaxine? It does the opposite-it pushes pressure up. Even other SNRIs are different. Duloxetine, another serotonin-norepinephrine drug, has a much milder effect on blood pressure. Desvenlafaxine, the active metabolite of venlafaxine, still raises it-even at low doses. So if you’ve tried one SNRI and had issues, the other likely won’t be much better. That’s why doctors often turn to venlafaxine only after SSRIs fail. It’s powerful for treatment-resistant depression. But that power comes with a cost: your heart and arteries pay attention to it.Who’s at Risk?
You might think, “I’m young and healthy-this won’t happen to me.” But that’s exactly what the 23-year-old in the case study thought. Risk isn’t just about age or preexisting conditions. It’s about your body’s sensitivity to norepinephrine. That said, some people are more vulnerable:- Those already on medication for high blood pressure-venlafaxine can make it harder to control
- People with heart disease, kidney problems, or a history of stroke
- Anyone taking other drugs that raise blood pressure (like decongestants, stimulants, or certain herbal supplements)
- Patients on doses above 150 mg/day
What You Should Do: Monitoring Guidelines
The American Psychiatric Association and Mayo Clinic agree: if you’re on venlafaxine, you need to check your blood pressure. Not once. Not just at the start. Regularly. Here’s what works:- Get your baseline BP before starting venlafaxine
- Check again at 2 weeks and 4 weeks after starting
- After that: monthly for the first 3 months if you’re on 150 mg or more
- Then every 3 months, or more often if your BP is rising
What If Your Blood Pressure Goes Up?
If your numbers climb, don’t panic. But don’t ignore it either. Most cases are reversible. The standard approach:- Reduce your dose-sometimes even a small drop (e.g., from 150 mg to 75 mg) helps
- If that doesn’t work, switch to a different antidepressant (SSRIs are usually safer for BP)
- Stop venlafaxine completely if your BP stays high or keeps climbing
What the Experts Say
Dr. Arif Khan, who led the landmark 2005 study on venlafaxine and blood pressure, says: “Concern about blood pressure shouldn’t stop you from using this drug if it’s helping your depression.” He’s right-but only if you’re monitoring. Dr. Costas Kosmas, who reviewed the cardiovascular risks in 2021, adds a darker note: “We’ve seen cases of posterior reversible encephalopathy syndrome (PRES)-a brain condition caused by sudden high blood pressure-after starting venlafaxine.” PRES can cause seizures, vision loss, and confusion. It’s rare, but it’s real. And it’s preventable. The FDA and European Medicines Agency both require warnings on venlafaxine labels. The FDA says: “Sustained blood pressure elevation has been observed.” The EMA says: “Regular monitoring is required.” That’s not a suggestion. It’s a rule.
Real Stories, Real Risks
Look at the data from patient forums:- On PsychForums, 68% of users reported higher blood pressure on venlafaxine
- 28% of negative reviews on Drugs.com mention BP issues
- One user said: “I thought it was just stress-until my pharmacist asked why I was taking a BP pill.”
What to Ask Your Doctor
Before you start-or if you’re already on it-ask these questions:- “What’s my baseline blood pressure, and what’s my target?”
- “Should I get a home monitor? Which one do you recommend?”
- “If my BP goes up, do we lower the dose first, or switch meds?”
- “Are there other antidepressants that won’t affect my blood pressure?”
- “What symptoms should I watch for? Headaches? Blurred vision? Chest pain?”
The Bottom Line
Venlafaxine works. For many people, it’s the only drug that lifts the fog of treatment-resistant depression. But it’s not harmless. Its effect on blood pressure is real, dose-dependent, and sometimes sudden. If you’re on venlafaxine, treat your blood pressure like a vital sign-not an afterthought. Check it. Track it. Talk about it. Your heart is counting on it.Can venlafaxine cause high blood pressure even at low doses?
Yes. While higher doses (above 150 mg/day) carry a greater risk, cases of severe hypertension have been documented even at 75 mg or 150 mg. One patient developed blood pressure of 210/170 mmHg on 150 mg/day with no prior history of hypertension. Individual sensitivity varies, so no dose is completely risk-free.
How long does it take for blood pressure to rise after starting venlafaxine?
It can happen anytime-from the first week to several months later. Most cases appear within the first 2 to 8 weeks, but some patients report gradual increases over 3 to 6 months. That’s why ongoing monitoring is essential, not just a one-time check.
Does venlafaxine affect everyone the same way?
No. Some people experience no change in blood pressure. Others see a small rise. A small percentage develop dangerous spikes. Genetics, metabolism, existing health conditions, and even diet can influence how your body reacts. There’s no way to predict who will be affected-so monitoring is critical for everyone.
Can I still take venlafaxine if I have high blood pressure?
Yes-but only if your blood pressure is well-controlled and you’re under close supervision. Venlafaxine doesn’t worsen controlled hypertension in most cases, but it can make it harder to manage. Your doctor will likely require more frequent BP checks and may adjust your antihypertensive meds accordingly.
What are the signs that venlafaxine is raising my blood pressure too much?
Symptoms include severe headaches, blurred vision, nosebleeds, chest pain, shortness of breath, dizziness, or confusion. These aren’t normal side effects-they’re warning signs of dangerously high blood pressure. If you experience any of these, check your BP immediately and contact your doctor or go to urgent care.
Will my blood pressure go back to normal if I stop venlafaxine?
In most cases, yes. Blood pressure typically returns to baseline within 1 to 4 weeks after stopping venlafaxine. However, never stop the medication abruptly without medical guidance. Your doctor will help you taper safely to avoid withdrawal symptoms like anxiety, nausea, or electric shock sensations.
Are there safer antidepressants for people concerned about blood pressure?
Yes. SSRIs like sertraline, escitalopram, and fluoxetine are generally considered safer for blood pressure. They rarely cause significant increases. If you have uncontrolled hypertension or heart disease, your doctor may recommend one of these instead. Duloxetine is another SNRI option, but it still carries some risk-just less than venlafaxine.



Jasmine Yule
December 30, 2025 at 19:40Okay but can we talk about how wild it is that doctors just hand this out like candy? I was on 75mg for 6 weeks and my BP shot up to 160/105-no symptoms, no warning. My pharmacist was the one who noticed I was buying OTC BP meds. They act like it’s ‘just a side effect’ like dry mouth. It’s not. It’s a silent grenade.
And why isn’t there a mandatory BP test before prescribing? This isn’t a vitamin. This is a drug that can literally kill you if you’re not paying attention.
Teresa Rodriguez leon
December 31, 2025 at 15:28I hate how people treat this like it’s a personal failure if your BP goes up. It’s not your fault. It’s the drug. I was on venlafaxine for 11 months and ended up in the ER with a 200/130 reading. No family history, no obesity, no caffeine. Just a pill that turned my body against me. They said ‘maybe try something else’ like it’s a fashion choice.
Manan Pandya
December 31, 2025 at 19:40The pharmacokinetic profile of venlafaxine is well-documented in relation to noradrenergic modulation. The dose-dependent norepinephrine reuptake inhibition (NRI) threshold at approximately 150 mg/day is consistent with clinical observations of elevated systolic and diastolic pressure. A meta-analysis by Khan et al. (2005) demonstrated a 2.3 mmHg mean increase in diastolic BP at therapeutic doses, with a 13% incidence of clinical hypertension above 300 mg/day. Monitoring is not optional-it is pharmacologically imperative.
Aliza Efraimov
December 31, 2025 at 22:54OMG I’m so glad someone finally said this. I was on venlafaxine and thought I was just ‘stressed’ until I passed out in the grocery store. My BP was 188/112. My doctor said ‘it’s probably anxiety’-NO. It was the drug. I cried for three days after I stopped it because I felt like I lost my mind… but then my BP went back to normal in 10 days. I’m never taking an SNRI again. If you’re on this, get a home monitor TODAY. Please. I don’t want anyone else to wake up in the ER like I did.
❤️🩹
Nisha Marwaha
January 2, 2026 at 11:54From a clinical pharmacology standpoint, the noradrenergic cascade induced by venlafaxine engages α1-adrenergic receptors in the vasculature, leading to vasoconstriction and increased peripheral resistance. This mechanism is distinct from SSRIs, which exhibit negligible affinity for norepinephrine transporters. Consequently, the hypertensive potential is a class effect of SNRIs, albeit with venlafaxine demonstrating the highest potency among them. Desvenlafaxine, despite being a metabolite, retains this liability. Therefore, baseline and serial BP assessments are non-negotiable in treatment algorithms.
Paige Shipe
January 3, 2026 at 00:15People act like this is some big secret. It's in the FDA label. It's in every prescribing guide. If you're not checking your BP, you're just being lazy. I've seen too many patients come in with stroke symptoms and say 'I didn't know it could do that.' Yes. It can. It does. Get a monitor. Track it. Don't be that person.
Tamar Dunlop
January 4, 2026 at 16:05As a Canadian clinician, I must emphasize the gravity of this issue within our public health framework. The Therapeutic Products Directorate mandates explicit cardiovascular monitoring for all patients initiated on venlafaxine, in accordance with Health Canada’s safety advisories. To neglect such monitoring is not merely an oversight-it is a breach of the standard of care. The human cost of underestimating this pharmacological risk is both measurable and tragically avoidable.
David Chase
January 5, 2026 at 00:50WHY DO PEOPLE STILL TAKE THIS?!?!?!!??!?!? I’ve seen 3 friends have strokes before 30 because of this damn drug. And the doctors? They’re just like ‘oh, maybe it’s stress’ while you’re having a seizure in the waiting room. This isn’t depression treatment-it’s a Russian roulette pill. If you’re on venlafaxine and you’re not checking your BP every week, you’re playing with your life. And if you’re a doctor prescribing it without a monitor? You’re a menace. 💀🩸血压警告!!!
Emma Duquemin
January 5, 2026 at 11:12Y’all, I was skeptical too-until my mom went from 118/76 to 190/110 on 150mg. She thought she was just getting ‘headaches from work.’ Turns out she was one migraine away from a hemorrhage. We got her a home monitor, she dropped to 75mg, and within 3 weeks, she was back to normal. I’m telling you-this isn’t hype. It’s survival. If you’re on this, treat your BP like your phone battery: check it daily. Don’t wait for the alarm to go off. You don’t get a second chance with your heart.
And yes, I’m still mad at the doctor who didn’t warn us. 😤
Kevin Lopez
January 7, 2026 at 09:02SNRI = hypertension risk. SSRIs = safer. Dose >150mg = high risk. Monitor or quit. Simple.