Venlafaxine Blood Pressure Risk Calculator
Your Blood Pressure Risk Assessment
This tool helps you understand your risk of blood pressure changes while taking venlafaxine based on the latest research.
Your Risk Assessment
Recommended Actions
Note: This calculator is for informational purposes only and is not a substitute for professional medical advice. Always consult with your healthcare provider for personalized guidance.
Based on clinical studies including the 2005 meta-analysis of 3,700+ patients and other documented cases.
When you start taking venlafaxine for depression or anxiety, you’re probably focused on how it helps your mood - not your blood pressure. But here’s the thing: venlafaxine can raise your blood pressure, sometimes significantly, even if you’ve never had high blood pressure before. This isn’t a rare side effect. It’s a well-documented, dose-dependent risk that doctors and patients need to take seriously.
How Venlafaxine Affects Blood Pressure
Venlafaxine, sold under brand names like Effexor and Effexor XR, is an SNRI - a serotonin-norepinephrine reuptake inhibitor. That means it boosts two brain chemicals: serotonin and norepinephrine. Serotonin helps with mood. Norepinephrine? It’s your body’s natural adrenaline. It increases heart rate, tightens blood vessels, and pushes blood pressure up.
At low doses (under 150 mg/day), venlafaxine acts mostly on serotonin. But once you hit 150 mg or higher, the norepinephrine effect kicks in hard. That’s when blood pressure changes start showing up. Research from a 2005 meta-analysis of over 3,700 patients found that at doses above 300 mg/day, about 13% of people developed clinically high diastolic blood pressure - more than double the rate of those on placebo.
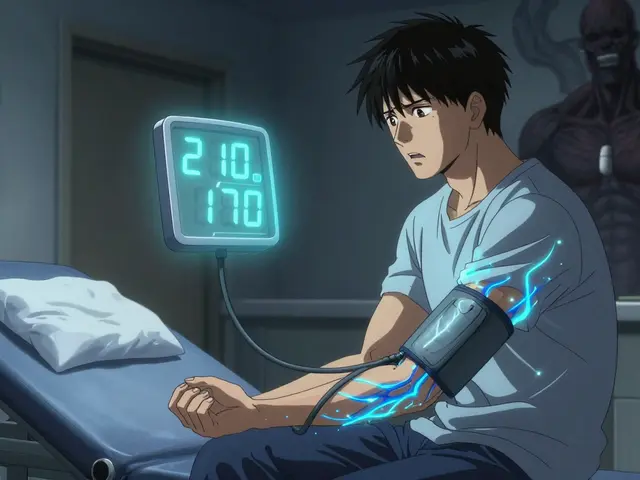
It’s not just about high doses. A 2014 case report described a 23-year-old man with no history of hypertension who developed blood pressure readings of 210/170 mmHg after just 10 months on 150 mg/day. That’s a hypertensive crisis - a medical emergency. His BP dropped back to normal within weeks after stopping the drug. This shows venlafaxine doesn’t always follow the rules. Some people are just more sensitive.
How Common Is High Blood Pressure With Venlafaxine?
Let’s break it down with real numbers:
- At doses under 150 mg/day: Blood pressure increases are usually mild - around 1-3 mmHg diastolic.
- At doses above 300 mg/day: Up to 13% of patients develop significant hypertension (diastolic >90 mmHg).
- On average, long-term use can raise diastolic BP by up to 15 mmHg.
- According to patient forums and drug review sites, about 28% of negative reviews mention high blood pressure as a concern.
- The NHS reports that up to 1 in 10 people experience high blood pressure as a side effect.
Compare that to SSRIs like sertraline or fluoxetine - they rarely affect blood pressure at all. Even other SNRIs like duloxetine have less impact. Venlafaxine stands out for its strong noradrenergic effect, and that’s exactly why it works well for treatment-resistant depression - but also why it carries this risk.
Who’s at Highest Risk?
Not everyone gets high blood pressure on venlafaxine. But some people are more vulnerable:
- Those taking doses above 150 mg/day - the risk climbs sharply.
- People with pre-existing high blood pressure - even though studies show venlafaxine doesn’t make existing hypertension worse, it can push it into dangerous territory.
- Patients with heart disease, kidney problems, or a history of stroke.
- Those who are genetically sensitive to norepinephrine - we’re still learning who these people are, but case reports suggest it happens.
- Older adults - their blood vessels are less flexible, and their bodies process drugs differently.
Interestingly, some patients with uncontrolled hypertension report that venlafaxine actually stabilized their BP. That’s rare, but it shows individual responses vary. Still, you can’t rely on that. Monitoring is non-negotiable.

What Symptoms Should You Watch For?
High blood pressure doesn’t always cause symptoms - which is why it’s called the silent killer. But when it spikes suddenly, you might notice:
- Severe headache, especially at the back of the head
- Nosebleeds (as seen in the 2014 case report)
- Blurred vision or seeing spots
- Chest pain or tightness
- Shortness of breath
- Confusion or dizziness
If your systolic BP hits 180 mmHg or higher, or your diastolic BP is over 110 mmHg, that’s a hypertensive emergency. Don’t wait. Call emergency services or go to the ER. This can lead to stroke, heart attack, or posterior reversible encephalopathy syndrome (PRES) - a rare but serious brain condition linked to sudden BP spikes.
Monitoring Guidelines: What Your Doctor Should Do
It’s not enough to just get a baseline reading. You need a plan.
The American Psychiatric Association and Mayo Clinic both recommend:
- Check blood pressure before starting venlafaxine.
- Measure again at 2 weeks and 4 weeks after starting or increasing the dose.
- For doses above 150 mg/day: Monitor monthly for the first 3 months, then every 3 months.
- For anyone over 65 or with cardiovascular risk factors: Check every 4-6 weeks, regardless of dose.
Home blood pressure monitors are a great tool. Take readings at the same time each day, sit quietly for 5 minutes before measuring, and keep a log to share with your doctor. Don’t wait for your next appointment if you feel something’s off.
What Happens If Your Blood Pressure Goes Up?
If your BP rises but stays below 140/90 mmHg, your doctor might just keep monitoring. No need to panic.
If it climbs above 140/90 mmHg:
- Dose reduction is the first step. Lowering from 225 mg to 150 mg often brings BP back down.
- Switching to another antidepressant - like an SSRI or bupropion - may be necessary.
- Stopping venlafaxine usually leads to BP normalization within 1-4 weeks.
- In rare cases, antihypertensive medication may be needed temporarily.
Never stop venlafaxine cold turkey. Tapering under medical supervision prevents withdrawal symptoms like brain zaps, nausea, and rebound anxiety.
Venlafaxine vs. Other Antidepressants: The Cardiovascular Trade-Off
Here’s how venlafaxine stacks up against other common antidepressants:
| Medication | Class | Typical BP Effect | Notes |
|---|---|---|---|
| Venlafaxine | SNRI | Increases (dose-dependent) | Strongest norepinephrine effect among SNRIs |
| Desvenlafaxine | SNRI (metabolite) | Increases (mild to moderate) | Similar to venlafaxine but less steep rise |
| Duloxetine | SNRI | Mild increase | Lower risk than venlafaxine |
| Sertraline | SSRI | Neutral or slight decrease | Safest for patients with hypertension |
| Fluoxetine | SSRI | Neutral | Very low risk |
| Imipramine | TCA | Variable - can cause hypotension or hypertension | Higher risk of arrhythmias and orthostatic drops |
| Bupropion | NDRI | Mild increase | Good alternative for treatment-resistant depression |
Venlafaxine is more effective than SSRIs for some people - especially those with fatigue, low energy, or treatment-resistant depression. But if you have high blood pressure, or even borderline readings, an SSRI might be safer to start with.
What’s the Bottom Line?
Venlafaxine is a powerful tool for depression and anxiety. But it’s not a first-choice drug for everyone. If you’re considering it:
- Ask your doctor for a baseline blood pressure reading.
- Get your BP checked at 2 and 4 weeks after starting or changing the dose.
- Keep a log - even small increases matter.
- Know the warning signs of dangerously high BP.
- If your BP rises, don’t panic - but don’t ignore it either.
For many, venlafaxine works wonders without a single blood pressure issue. But for others, it’s a silent threat. The key isn’t avoiding the drug - it’s monitoring it like you would a prescription for insulin or blood thinners. Your mood matters. But so does your heart.
Can venlafaxine cause high blood pressure even at low doses?
Yes. While the risk increases significantly at doses above 150 mg/day, there are documented cases of severe hypertension occurring even at 75 mg or 150 mg. One case report described a 23-year-old man whose blood pressure spiked to 210/170 mmHg after 10 months on 150 mg/day. Individual sensitivity varies, and genetic factors may play a role. Never assume low doses are risk-free.
How long does it take for blood pressure to return to normal after stopping venlafaxine?
In most cases, blood pressure begins to drop within days of stopping venlafaxine and returns to baseline within 1 to 4 weeks. The exact timeline depends on how high it went, how long you were on the medication, and your overall health. If your BP was only mildly elevated, it may normalize in under a week. For severe cases, it can take longer, and sometimes temporary blood pressure medication is needed.
Should I avoid venlafaxine if I have high blood pressure?
Not necessarily. Venlafaxine doesn’t worsen controlled hypertension in most patients, according to clinical studies. But if your blood pressure is uncontrolled (above 140/90 mmHg), your doctor will likely start you on an SSRI like sertraline or fluoxetine first. If those don’t work and venlafaxine is needed, your BP must be closely monitored and managed with medication if necessary. It’s about risk vs. benefit - not an absolute yes or no.
Is desvenlafaxine safer for blood pressure than venlafaxine?
Desvenlafaxine (Pristiq) is the active metabolite of venlafaxine and has similar effects, but the blood pressure rise tends to be slightly less pronounced. Studies show it causes a 0.66-3.41 mmHg increase in diastolic BP, compared to up to 15 mmHg with high-dose venlafaxine. It’s not risk-free, but for some patients, it may be a gentler option. Still, monitoring is required for both.
Can I take blood pressure medication with venlafaxine?
Yes, many patients take both safely. Common blood pressure medications like ACE inhibitors, calcium channel blockers, or beta-blockers can be used alongside venlafaxine. Your doctor will check for interactions - for example, beta-blockers can sometimes mask anxiety symptoms that venlafaxine is meant to treat. But combining them is often the best way to manage both depression and hypertension without compromising either.
Are there any natural ways to lower blood pressure while on venlafaxine?
Lifestyle changes help - but they’re not a substitute for medical monitoring. Reducing sodium, exercising regularly, limiting alcohol, managing stress, and maintaining a healthy weight can all support normal blood pressure. However, if venlafaxine is causing a significant rise, these changes alone won’t reverse it. Don’t rely on supplements like magnesium or garlic - there’s no strong evidence they counteract venlafaxine-induced hypertension. Always talk to your doctor before adding anything.
What should I do if I forget to check my blood pressure for a few weeks?
Don’t panic, but don’t ignore it either. If you’ve missed a scheduled check, get your BP measured as soon as possible. If you’re feeling fine and have no symptoms, it’s likely okay - but you should reschedule your next checkup and set a reminder. If you’ve had symptoms like headaches, nosebleeds, or dizziness, go to your doctor immediately. Missing a check doesn’t mean you’re in danger - but it does mean you’re flying blind.
Final Thoughts
Venlafaxine saves lives. It helps people who’ve tried everything else. But it’s not a gentle drug. Its power comes with responsibility - for you and your doctor. If you’re on venlafaxine, treat your blood pressure like a vital sign, not an afterthought. Keep a log. Ask questions. Speak up if something feels off. The goal isn’t just to feel better emotionally - it’s to stay healthy physically, too.




Fabian Riewe
December 29, 2025 at 15:35Man, I’ve been on venlafaxine for 3 years at 225mg and my BP’s been perfect - 118/76. But I check it every week like clockwork with my home monitor. Seriously, if you’re on this stuff, treat it like you’re on warfarin. No excuses. I used to forget, then had a weird headache one day - turned out my diastolic was 98. Scared the crap outta me. Now I log it in my phone. Simple as that.
Also, if your doc doesn’t bring it up, ask. They’re busy. You’re the one living with it.
Nicole K.
December 30, 2025 at 17:07This is why people shouldn’t take antidepressants unless they’re desperate. You’re trading one problem for another. Your heart shouldn’t have to pay for your mood. I’d rather be sad than have a stroke.
Sharleen Luciano
December 31, 2025 at 19:38How is this even a topic? Anyone with a basic understanding of pharmacology knows SNRIs elevate norepinephrine, and norepinephrine = vasoconstriction. The real question is why aren’t more patients being screened proactively? I’ve seen clinicians prescribe this like it’s vitamin D. Pathetic.
Also, if you’re using home monitors, make sure they’re validated. Most $20 Amazon ones are garbage. Get an Omron. Or don’t bother.
Joe Kwon
January 2, 2026 at 12:12As someone who’s been on both venlafaxine and desvenlafaxine, I’ll say this: the BP spike on venla is real, but it’s not inevitable. I went from 150mg venla (BP 148/92) to 100mg desvenlafaxine - BP dropped to 122/78 in 3 weeks. Same efficacy on my depression, zero headaches, no zaps. The key is not avoiding SNRIs - it’s optimizing the *type*. Desvenlafaxine has a cleaner PK profile, less peak-to-trough fluctuation, and frankly, less cardiovascular noise.
Also, if you’re over 50 and on >150mg, get a 24-hour ambulatory BP monitor. It’s not optional. Out-of-office readings tell the real story. Clinic readings are often white-coat noise.
Lisa Dore
January 4, 2026 at 07:20Hey, if you’re reading this and you’re scared - you’re not alone. I was terrified when my BP jumped after starting venlafaxine. But my psychiatrist and my primary care doc worked together. We lowered the dose, added a low-dose beta-blocker, and I started walking 30 mins a day. Now my BP’s normal and I’m actually sleeping better than I have in years.
Don’t quit the med unless you have to. Just don’t ignore the numbers. You’re not weak for needing help with this. You’re smart for paying attention.
Himanshu Singh
January 5, 2026 at 17:32in india most doc dont even check bp before prescibing venla... i had to buy my own monitor. now i check every 3 days. my bp was 150/95 at 150mg, now at 75mg its 125/80. its not perfect but i can live with it. thanks for the post!
Greg Quinn
January 6, 2026 at 15:57It’s fascinating how we treat mental health meds like they exist in a vacuum - as if the body doesn’t have to pay the price for chemical balance. Venlafaxine doesn’t just ‘help your mood.’ It hijacks your autonomic nervous system. The fact that we don’t routinely treat BP as a core vital sign with these drugs says more about our medical culture than it does about the drug itself.
Maybe the real question isn’t ‘Can venlafaxine raise BP?’ - but ‘Why do we accept trade-offs like this as normal?’ We wouldn’t let someone take a steroid for depression without monitoring glucose. Why is BP any different?
Amy Cannon
January 6, 2026 at 18:53Thank you for this comprehensive, deeply informative piece - it is truly a masterclass in clinical communication. As someone who has spent decades in healthcare administration in the Pacific Northwest, I must commend the meticulous attention to pharmacokinetic nuance and the ethically grounded emphasis on patient autonomy. I particularly appreciated the inclusion of the 2014 case report - it exemplifies the necessity of individualized care in an era of algorithmic medicine.
That said, I do have a minor quibble: the table formatting appears to have been rendered imperfectly in some browsers, possibly due to HTML5 compatibility issues with legacy mobile clients. Perhaps a markdown alternative or a downloadable PDF appendix would enhance accessibility? Also, I noticed a typo in the NHS stat - it reads ‘1 in 10’ but I believe the actual figure is closer to 1 in 8 based on the 2017 NICE guidelines. Just a thought - your work deserves perfection.
And yes, I do use a Withings BPM Core - it syncs to Apple Health and even does ECG now. Highly recommend.