EHR integration connects pharmacies and providers to improve prescription safety, reduce errors, and cut hospital readmissions. Learn how it works, why most pharmacies still lack it, and what’s changing in 2025.
Pharmacy EHR: What It Is and How It Changes Patient Care
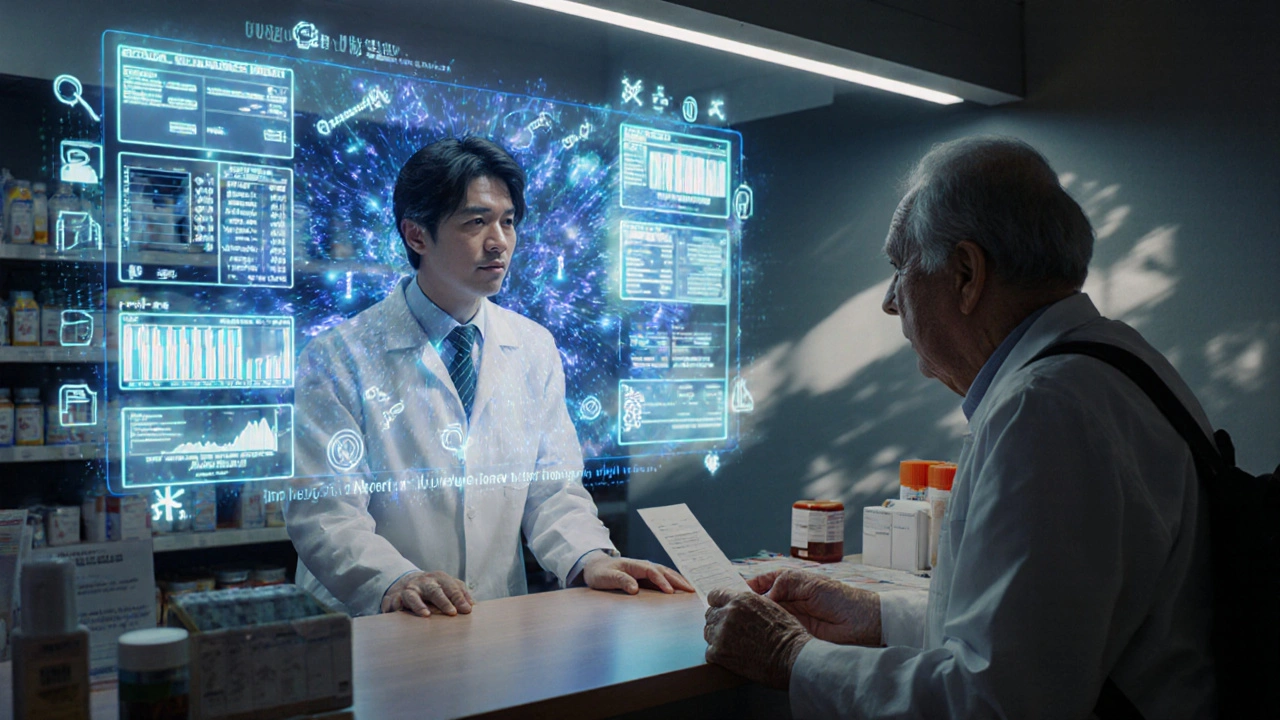
When you hear pharmacy EHR, an electronic system that stores and shares a patient’s medication history, prescription data, and allergy alerts between pharmacists and other providers. Also known as electronic pharmacy records, it’s not just a digital file cabinet—it’s a live safety net that prevents dangerous drug overlaps and keeps your treatment on track. Most people think of EHRs as something doctors use, but pharmacy EHRs are the quiet backbone of safe medication use. They’re what let your pharmacist know you’re on blood thinners before filling a new painkiller, or spot that your antidepressant clashes with your blood pressure med—even if your doctor didn’t catch it.
Pharmacy EHRs don’t work alone. They connect with electronic health records, the broader digital health systems used by hospitals and clinics to track diagnoses, lab results, and treatment plans. This link means your pharmacist sees your recent hospital discharge summary or a new diabetes diagnosis, so they can adjust your meds before you even walk in. They also tie into medication management, the process of reviewing all your drugs to avoid duplicates, side effects, or gaps in care. This isn’t just about counting pills—it’s about understanding how your entire drug stack affects your kidneys, your heart, your mood, and your ability to sleep. Without this integration, mistakes happen. A patient on warfarin gets a new antibiotic that spikes their INR. Someone with kidney disease gets a dose of metformin that’s too high. These aren’t rare cases—they’re preventable, and pharmacy EHRs are built to stop them.
And it’s not just about safety. Pharmacy EHRs help cut down on paperwork, reduce refill delays, and give you more time with your pharmacist instead of waiting on hold. They flag when a generic isn’t working for you, so your provider can appeal an insurance denial. They track adherence—so if you haven’t picked up your statin in three months, your pharmacist can reach out before you have a heart attack. This system doesn’t replace human judgment; it makes it sharper. Whether you’re managing chronic pain, dealing with multiple prescriptions, or just trying to avoid a bad reaction, pharmacy EHRs are working behind the scenes to keep you safe.
Below, you’ll find real-world guides on how these systems affect your care—from reporting dangerous side effects to the FDA, to fighting insurance denials for brand-name drugs, to understanding how your copays stack up against your out-of-pocket max. These aren’t abstract tech talks. They’re the practical consequences of how pharmacy EHRs shape what you pay, what you get, and how well you’re protected.