SSRI-NSAID Risk Calculator
This calculator estimates your risk of gastrointestinal bleeding when taking both an SSRI and an NSAID. Based on clinical evidence, combining these medications increases bleeding risk by up to 75% compared to NSAIDs alone. Use this tool to understand your risk and make safer medication decisions.
Enter your information and click "Calculate Risk" to see your personalized assessment.
When you're managing chronic pain and depression at the same time, it's easy to assume that taking an SSRI and an NSAID together is just another routine part of your daily pills. But this common combo carries a hidden danger-one that many doctors still overlook and most patients never hear about. SSRIs with NSAIDs can dramatically increase your risk of serious, even life-threatening, gastrointestinal bleeding. This isn’t a rare side effect. It’s a well-documented, predictable interaction that affects tens of thousands of people every year in the U.S. alone.
Why This Combo Is So Dangerous
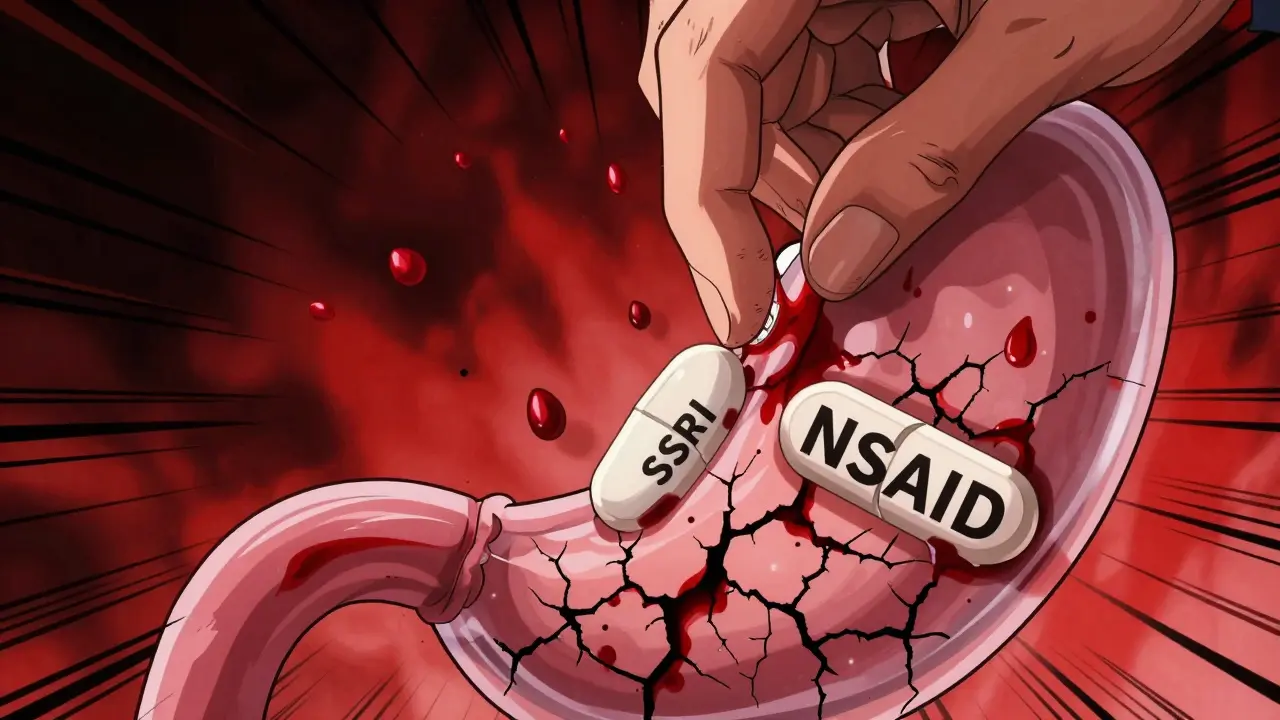
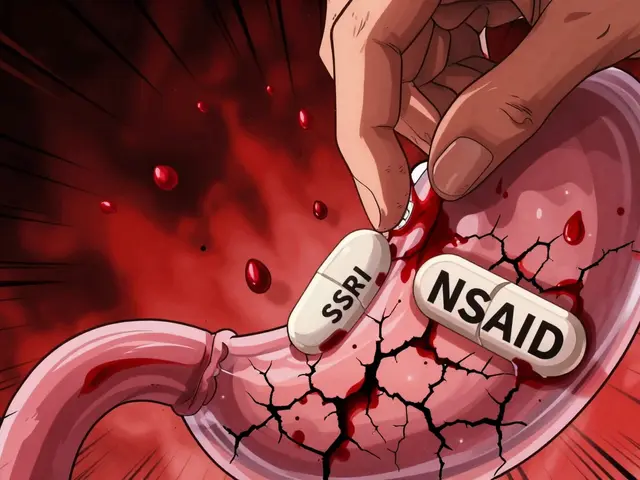
SSRIs like sertraline, fluoxetine, and escitalopram work by boosting serotonin in your brain to lift your mood. But serotonin isn’t just a mood chemical-it’s also critical for blood clotting. Platelets, the cells that stop bleeding, rely on serotonin to stick together and form clots. SSRIs block the serotonin transporter on platelets, which means they can’t grab enough serotonin to do their job properly. Your blood starts to thin-not as much as warfarin or aspirin, but enough to matter. NSAIDs like ibuprofen, naproxen, and diclofenac are even more direct. They attack the stomach lining, reducing protective prostaglandins and making it easier for acid to burn through. They also interfere with platelet function, just like SSRIs, but through a different pathway. When you take both, you’re not just adding two risks-you’re multiplying them. Studies show the combination increases your risk of upper GI bleeding by 75% compared to using NSAIDs alone. That’s not a small bump. That’s a major jump.The Numbers Don’t Lie
A 2022 meta-analysis published in Nature Scientific Reports reviewed data from over 1.2 million patients and found a consistent odds ratio of 1.75 for GI bleeding with SSRI-NSAID use. That means if 1 in 100 people on NSAIDs alone have a bleed in a year, then 1.75 in 100 people on both drugs will. Multiply that across millions of prescriptions, and you’re looking at thousands of preventable hospitalizations annually. Even more alarming: a 2002 JAMA Internal Medicine study found that people on both drugs had more than a 12-fold higher risk of bleeding compared to people taking neither. That risk spikes even higher if you’re over 65, have a history of ulcers, or are also taking low-dose aspirin. In fact, combining all three-SSRI, NSAID, and aspirin-creates a perfect storm. The bleeding risk becomes comparable to that of full anticoagulants like warfarin.Not All NSAIDs Are Created Equal
If you need pain relief while on an SSRI, not all NSAIDs are equally risky. Celecoxib, a COX-2 selective inhibitor, has been shown to carry the lowest GI bleeding risk among NSAIDs. It doesn’t suppress stomach-protecting prostaglandins as much as older NSAIDs. But even celecoxib isn’t risk-free when paired with SSRIs. Among non-selective NSAIDs, ibuprofen tends to be slightly safer than naproxen or diclofenac, especially at lower doses. But here’s the catch: the risk isn’t just about which drug you take-it’s about how long and how often you take it. Using NSAIDs for more than 90 days or at doses above 1,200 mg of ibuprofen equivalent per day significantly raises your chances of bleeding. Short-term use for a sprained ankle? Lower risk. Daily use for arthritis? High risk.
What About Acetaminophen?
If you need pain relief and you’re on an SSRI, acetaminophen (also called paracetamol) is your safest bet. Unlike NSAIDs, it doesn’t affect platelets or the stomach lining. Multiple studies, including the 2023 Haghbin et al. meta-analysis, show no increased bleeding risk when acetaminophen is used with SSRIs. It’s not as strong for inflammation, but for headaches, muscle aches, or joint pain without swelling, it works just fine. Many patients don’t realize this. On patient forums like Reddit and Drugs.com, over 28% of users on SSRI-NSAID combos report GI issues, and 12% say they had actual bleeding episodes-often after months of use. One common story: “I was on sertraline and ibuprofen for six months before I ended up in the ER with internal bleeding. No one ever warned me.”What Doctors Should Do
The American Gastroenterological Association (AGA) has clear guidelines: if you must take both an SSRI and an NSAID, you need a proton pump inhibitor (PPI) like omeprazole or pantoprazole. PPIs reduce stomach acid and help heal the lining, cutting the bleeding risk by about 70%. That’s not a small win-it’s a game-changer. But here’s the problem: many prescribers don’t think to ask about NSAID use when starting an SSRI. And many patients don’t think to mention their daily ibuprofen for back pain. A 2021 study showed that after clinician education programs, inappropriate SSRI-NSAID combinations dropped from 28% to just 9% in primary care clinics. That’s proof that awareness works. For high-risk patients-those over 65, with prior ulcers, or on blood thinners-the rule is simple: avoid NSAIDs entirely. Use acetaminophen. Try physical therapy. Consider topical NSAIDs (gels or patches), which have minimal systemic absorption. If you absolutely must use an oral NSAID, pair it with a PPI and monitor closely.
Real-World Consequences
The financial and human cost is massive. In the U.S., SSRI-NSAID related GI bleeds cost an estimated $1.2 billion per year. That includes $842 million for hospital stays, $217 million for ER visits, and $143 million for follow-up care. The FDA received over 8,400 adverse event reports between 2010 and 2020-but experts believe that’s only 1-10% of actual cases. Worse, many patients aren’t diagnosed quickly. A 2021 Medscape case report described a 68-year-old man who needed three blood transfusions before doctors realized his stomach bleed was caused by fluoxetine and naproxen. He’d been taking both for over a year.What You Can Do Right Now
If you’re on an SSRI and regularly take NSAIDs, here’s what to do:- Stop taking NSAIDs unless your doctor says it’s absolutely necessary.
- Switch to acetaminophen for pain relief. It’s safe with SSRIs.
- If you have chronic pain, ask about non-drug options: physical therapy, heat/cold therapy, acupuncture.
- If you must continue NSAIDs, ask for a PPI (omeprazole 20 mg daily is common).
- Tell every new doctor you see that you’re on an SSRI. Don’t assume they’ll check your med list.
- Watch for warning signs: black or tarry stools, vomiting blood, dizziness, weakness, or sudden abdominal pain.
The Future Is Changing
Hospitals and clinics are starting to catch up. New EHR systems now include automated alerts when an SSRI and NSAID are prescribed together. The GI-BLEED risk calculator, launched in 2023, uses 12 factors-including your age, specific medications, and genetic metabolism-to give you a personalized risk score. It’s accurate 89% of the time. Research is also exploring safer antidepressants. Vortioxetine, a newer drug, showed 40% fewer bleeding events than traditional SSRIs in a 2022 trial. And future NSAID formulations may target only inflamed joints, avoiding the stomach entirely. By 2030, experts predict a 60% drop in inappropriate SSRI-NSAID prescribing thanks to better alerts, patient education, and safer alternatives. But that doesn’t mean you should wait. The risk is real today. The solution is simple: don’t combine them unless you absolutely have to-and if you do, protect your stomach.Can I take ibuprofen with sertraline?
You can, but it’s not safe without protection. Combining ibuprofen with sertraline increases your risk of stomach bleeding by 75% compared to using ibuprofen alone. If you need pain relief, switch to acetaminophen. If you must use ibuprofen, take a proton pump inhibitor like omeprazole daily to protect your stomach lining.
Which SSRI has the lowest bleeding risk?
Sertraline and citalopram appear to have slightly lower bleeding risk than fluoxetine or paroxetine because they’re weaker at blocking serotonin reuptake in platelets. But the difference isn’t large enough to rely on. The real issue is the combination with NSAIDs, not the specific SSRI. Avoid NSAIDs altogether if possible.
Is it safe to take SSRIs with Tylenol?
Yes. Acetaminophen (Tylenol) does not affect platelets or the stomach lining, so it doesn’t increase bleeding risk when taken with SSRIs. It’s the preferred pain reliever for people on antidepressants. Use it for headaches, muscle aches, or mild arthritis pain.
What are the signs of GI bleeding from SSRIs and NSAIDs?
Watch for black, tarry stools (melena), vomiting blood or material that looks like coffee grounds, sudden dizziness, weakness, rapid heartbeat, or sharp abdominal pain. These are signs of internal bleeding. If you experience any of these, seek emergency care immediately.
Should I stop my SSRI if I need NSAIDs?
Don’t stop your SSRI without talking to your doctor. Stopping abruptly can cause withdrawal symptoms. Instead, ask your doctor to help you switch from NSAIDs to acetaminophen or another pain relief option. If you need the NSAID for a short time, use a PPI and monitor closely. Never combine them without a plan.
How long does it take for bleeding risk to go up?
Risk increases with duration. Studies show the highest risk occurs after 90 days of combined use, but bleeding can happen anytime-even within weeks. There’s no safe window. The longer you take both drugs together, the higher your risk becomes. That’s why prevention should start on day one.



Hannah Taylor
December 21, 2025 at 11:21lol so now the FDA is gonna ban ibuprofen? 🤡 they’ve been hiding this since 2002 but no one cared until big pharma realized they could sell more PPIs. i’ve been on sertraline and naproxen for 8 years. no bleed. no hospital. just a guy who knows his body better than some study in nature.
Cara C
December 22, 2025 at 09:06this is such an important post. i had no idea combining my antidepressant with my nightly ibuprofen for back pain was this dangerous. switched to tylenol last week and already feel better-no more stomach nausea. thank you for sharing the science and not just fear.
Grace Rehman
December 24, 2025 at 06:46so we’re telling people to avoid NSAIDs because they thin blood and hurt the stomach… but we’re still okay with drinking alcohol which does both and then some? and no one screams about that? we live in a world where a pill gets a 12-page warning label but a bottle of whiskey gets a ‘drink responsibly’ sticker. logic is dead
Orlando Marquez Jr
December 24, 2025 at 15:37The confluence of pharmacological interactions and clinical oversight represents a significant public health challenge. Empirical data from longitudinal cohort studies substantiate the elevated risk profile associated with concurrent SSRI and NSAID administration. It is imperative that prescribers engage in comprehensive medication reconciliation.
Jackie Be
December 25, 2025 at 16:26I WAS ON SERTRALINE AND IBUPROFEN FOR 14 MONTHS AND I ALMOST DIED. BLACK STOOLS. DIZZINESS. I THOUGHT I WAS JUST ANEMIC. NO ONE TOLD ME. NOW I TAKE TYLENOL AND I’M ALIVE. YOU NEED TO READ THIS. PLEASE.
John Hay
December 27, 2025 at 13:12This isn’t complicated. If you’re on an SSRI and you’re taking NSAIDs daily, you’re playing Russian roulette with your gut. Stop. Use acetaminophen. Ask for a PPI. That’s it. No drama. No exceptions. Your stomach doesn’t care about your workout routine.
Jon Paramore
December 28, 2025 at 10:28The COX-1 inhibition by non-selective NSAIDs synergizes with platelet 5-HT transporter blockade by SSRIs, resulting in impaired primary hemostasis. The OR of 1.75 for upper GI bleed is statistically significant (p<0.001). PPI co-prescription reduces risk by ~70% via mucosal acid suppression. Acetaminophen remains first-line for analgesia in this cohort.
Swapneel Mehta
December 29, 2025 at 04:28I’m from India and we use ibuprofen with antidepressants all the time here. No one talks about bleeding. Maybe it’s because we don’t have access to PPIs or regular checkups. But I’m glad someone’s raising awareness. Maybe this will change things.
Cameron Hoover
December 29, 2025 at 14:01I used to take naproxen for my arthritis and sertraline for anxiety. I didn’t think twice. Then one morning I passed out. Turns out I lost two units of blood. I didn’t even know I was bleeding. Now I use heat packs and cryotherapy. It’s not magic, but it’s safer. Don’t wait until you’re in the ER.
Stacey Smith
December 30, 2025 at 15:16This is why America is weak. We medicate everything instead of just pushing through pain. You want to feel better? Stop being a baby. Take your ibuprofen. Stop whining about stomach lining. We used to be tougher.
Ben Warren
January 1, 2026 at 11:26The systemic failure in primary care prescribing practices is both lamentable and preventable. The conflation of patient autonomy with clinical negligence results in avoidable morbidity. The absence of mandatory pharmacovigilance protocols in electronic health records constitutes a gross dereliction of duty by institutional stakeholders. One cannot ethically prescribe a dual-risk regimen without concurrent gastroprotection. The data are unequivocal. The silence is complicity.
Teya Derksen Friesen
January 3, 2026 at 05:36I appreciate the depth of this post. As a pharmacist in Canada, I’ve seen this exact scenario play out too often. Patients assume their doctor knows all their meds. They don’t mention the Advil they take for headaches. We need better systems-not just more warnings. Maybe a mandatory pop-up in EHRs when SSRIs and NSAIDs are prescribed together? We’ve done it for opioids. Why not this?