Living with IBS-Mixed means your gut feels like it’s on a rollercoaster-one day you’re stuck, the next you’re rushing to the bathroom. It’s not just inconvenient; it’s exhausting. You try to eat normally, but fear creeps in before every meal. You cancel plans because you don’t know if your body will cooperate. And no matter what you do, the meds that help one symptom make the other worse. You’re not alone. About one in five people with IBS experience this back-and-forth between constipation and diarrhea. It’s called IBS-Mixed, or IBS-M, and it’s the most complex subtype to manage.
What Exactly Is IBS-Mixed?
IBS-Mixed isn’t just "IBS that acts up sometimes." It’s a specific diagnosis with clear rules. According to the Rome IV criteria (used by doctors worldwide), you’re diagnosed with IBS-M if you’ve had abdominal pain at least once a week for the past three months, and your bowel habits show a clear pattern: at least 25% of your stools are hard or lumpy (Bristol Stool Scale types 1-2), and at least 25% are loose or watery (types 6-7). That means you’re not just having occasional changes-you’re regularly switching between two extremes.
Unlike Crohn’s or ulcerative colitis, IBS-M doesn’t involve inflammation or damage to your intestines. Instead, it’s about how your gut functions. Your nerves are overly sensitive, your muscles contract irregularly, and the balance of bacteria in your gut is off. Stress makes it worse. Certain foods trigger it. And no, it’s not "all in your head." It’s a real, measurable condition affecting your nervous system and gut microbiome.
Why Is IBS-Mixed So Hard to Treat?
Here’s the catch: what helps constipation often makes diarrhea worse, and vice versa. Take laxatives-they might get you moving, but they can turn a mild episode into a full-blown flare. Loperamide (Imodium) calms diarrhea, but if you take it during a constipation phase, you’re stuck. That’s why so many people with IBS-M end up cycling through meds, feeling frustrated and confused.
Studies show that single-target drugs like linaclotide (for constipation) or eluxadoline (for diarrhea) only help about 20% of IBS-M patients. That’s half the success rate seen in IBS-C or IBS-D. The reason? Your body isn’t just constipated or just diarrheal-it’s both, at different times. You need a strategy that adapts.
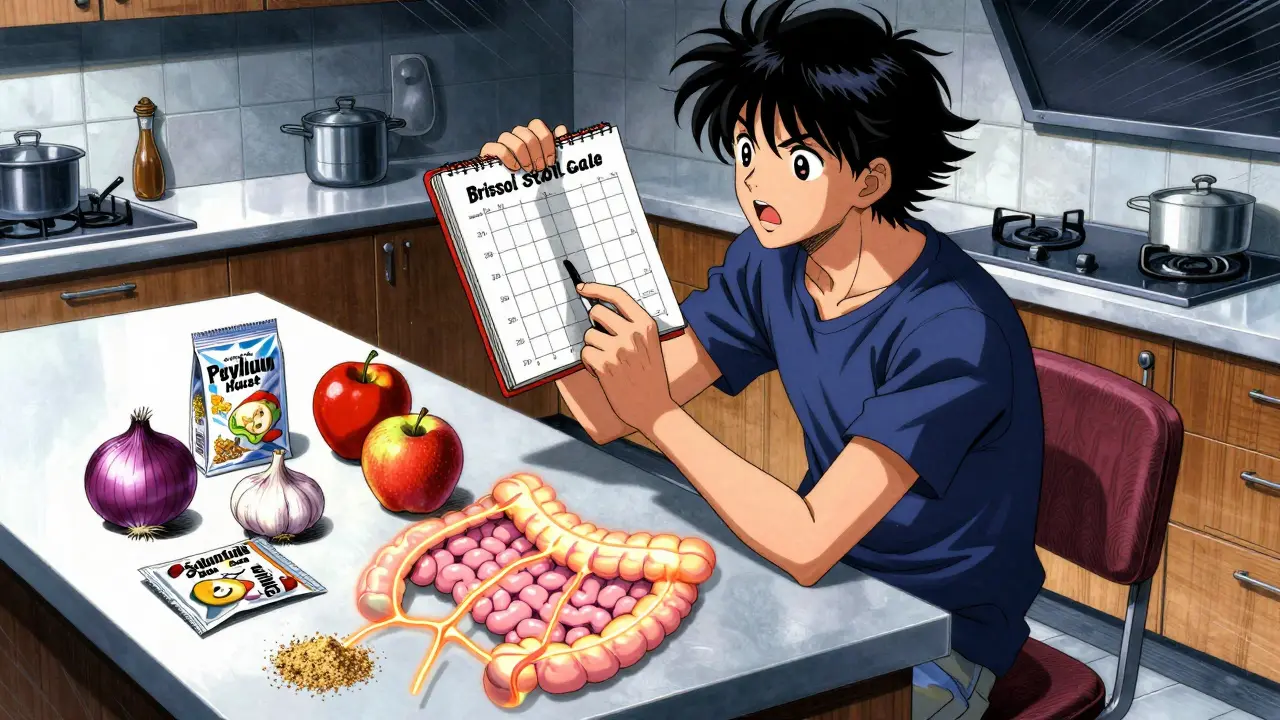
Food Is Your First Line of Defense
More than 70% of people with IBS-M see improvement with dietary changes. But not all diets work the same. The low FODMAP diet is the most researched-and it’s the one most people swear by. FODMAPs are short-chain carbs that ferment in your gut, pulling in water and causing gas. That’s bad news for someone with IBS-M.
The diet has three phases: elimination, reintroduction, and personalization. You cut out high-FODMAP foods like onions, garlic, wheat, apples, milk, and artificial sweeteners for 2-6 weeks. If your symptoms drop, you slowly add foods back in one at a time to find your triggers. A 2021 study in Gastroenterology found that 50-60% of IBS-M patients had significant relief on this diet. That’s lower than the 70-75% seen in IBS-D, but still a major win.
Real people report results. One user on Reddit said after three months of strict low FODMAP and daily peppermint oil capsules, her symptom days dropped from 25 to 8 per month. Others found relief with soluble fiber like psyllium husk-5 grams a day helps stabilize stools without triggering either extreme. But here’s the catch: you need a dietitian who knows IBS. Doing this alone often leads to over-restriction, nutrient gaps, and burnout.
Medications: The Balancing Act
There’s no magic pill for IBS-M. But having the right tools on hand can make a huge difference. Most successful plans involve keeping two medications ready:
- For constipation: Polyethylene glycol (Miralax) at 17g daily is gentle and doesn’t cause cramping. Magnesium citrate works fast but can be too strong-use it only during flare-ups.
- For diarrhea: Loperamide (Imodium) at 2-4mg as needed. Don’t take it daily. Use it only when you’re sure you’re in a diarrhea phase.
Antispasmodics like dicyclomine (10-20mg as needed) help with cramping and pain. They work equally well across all IBS types. And antidepressants? Yes, really. Low-dose tricyclics (like amitriptyline) or SSRIs (like sertraline) aren’t just for mood-they help regulate gut nerves. Studies show 55-60% of IBS-M patients respond better to antidepressants than to other meds. Why? Because they reduce pain signals and improve bowel control at the same time.
Enteric-coated peppermint oil (like IBgard) is another option. It relaxes gut muscles and reduces bloating. In Amazon reviews, 68% of IBS-M users reported less pain and 57% less bloating. A few complain of heartburn, but it’s generally well-tolerated.

Stress Isn’t Just a Trigger-It’s Part of the Problem
Stress doesn’t cause IBS-M, but it turns up the volume on every symptom. A 2019 study found 68% of IBS-M patients say stress makes their symptoms worse. That’s why therapy isn’t optional-it’s essential.
Cognitive behavioral therapy (CBT) is backed by 12 clinical trials. It doesn’t just teach you to relax. It rewires how your brain responds to gut signals. In one study, CBT cut symptom severity by 40-50%. That’s more than double the improvement from just learning about IBS. Apps like Cara Care offer guided CBT programs designed for IBS, and they’re now covered by some employers.
Even simple techniques help: diaphragmatic breathing for 5 minutes a day, daily walks, or journaling your symptoms and emotions. You don’t need to be a yoga master. You just need to interrupt the stress-gut cycle.
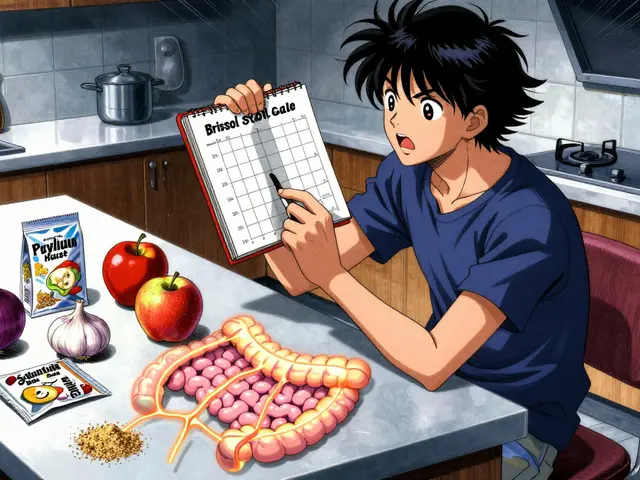
Tracking Is Non-Negotiable
If you don’t track your symptoms, you’re guessing. And guessing leads to frustration. You need to know what triggers what. Use a simple log: record your bowel movements (Bristol Scale), pain level (0-10), food eaten, stress level, and meds taken. Do this for at least four weeks.
People who use digital apps like Cara Care or Bowel Buddy see 35% better results than those using paper diaries. Why? Because patterns emerge. Maybe you notice pain spikes after coffee on weekends. Or bloating after eating avocado on Tuesdays. Once you see the pattern, you can adjust.
Don’t wait for your doctor to ask. Bring your log to every appointment. It shows you’re serious-and gives your doctor real data to work with.
What’s New in IBS-M Treatment?
The field is moving fast. In 2023, the FDA approved ibodutant, a new drug that targets gut nerve receptors. In phase 3 trials, it improved global symptoms in 45% of IBS-M patients-compared to 28% on placebo. It’s not on the market yet, but it’s a sign that researchers are finally focusing on IBS-M specifically.
Microbiome testing is also gaining ground. Companies like Viome use AI to analyze your gut bacteria and suggest personalized diets. In a 2023 pilot study, 58% of users saw symptom improvement. It’s expensive and not covered by insurance yet, but it’s a glimpse into the future: treatment tailored to your unique gut.
What Doesn’t Work (And Why)
Many people try quick fixes that backfire:
- Overusing laxatives: Leads to dependency and worsens diarrhea later.
- Going gluten-free without a diagnosis: Only helps if you have celiac disease. For most, it’s the FODMAPs in wheat-not gluten-that cause trouble.
- Eliminating entire food groups: You risk malnutrition and make recovery harder.
- Ignoring stress: Medications alone won’t fix it if your nervous system stays on high alert.
And yes, you’ll have setbacks. There’s no cure. But you can get to a point where symptoms are mild, predictable, and don’t control your life.
Getting Started: Your 30-Day Plan
Here’s what to do next:
- Download a symptom tracker app (Cara Care, Bowel Buddy, or even Google Sheets).
- Start a low FODMAP elimination diet for 4 weeks-cut out onions, garlic, wheat, dairy, apples, and artificial sweeteners.
- Take 5g of psyllium husk daily (mix in water) to stabilize stools.
- Keep loperamide and polyethylene glycol on hand, but use them only when needed.
- Try 5 minutes of deep breathing every morning.
- After 4 weeks, review your log. If symptoms improved, start reintroducing FODMAPs one at a time.
It takes 3-6 months to master this. Don’t expect perfection. Aim for progress. Most people who stick with it reduce their symptom days by half or more.
When to See a Specialist
If you’ve tried basic changes for 3 months with no improvement, see a gastroenterologist who specializes in IBS. Ask for:
- Tests to rule out celiac disease (blood test)
- CRP or ESR to check for inflammation
- A referral to a dietitian trained in low FODMAP
- Discussion of antidepressants or newer meds like ibodutant (when available)
You don’t have to live like this. IBS-M is complex, but it’s manageable. With the right tools, you can go from feeling out of control to feeling confident again.
Can IBS-Mixed turn into Crohn’s disease or ulcerative colitis?
No. IBS-M is a functional disorder-it doesn’t cause inflammation or damage to the gut lining. Crohn’s and ulcerative colitis are inflammatory diseases with visible changes in the intestine. Blood tests and stool markers can easily tell the difference. If your doctor has ruled out those conditions, you don’t need to worry about IBS-M turning into them.
Is the low FODMAP diet permanent?
No. The elimination phase lasts 2-6 weeks. After that, you systematically reintroduce FODMAPs to find your personal triggers. Most people end up eating a modified low FODMAP diet long-term, not a full restriction. The goal is to expand your food choices safely, not to eliminate everything forever.
Why do some people say peppermint oil helps, but others get heartburn?
Regular peppermint oil can relax the lower esophageal sphincter, causing acid reflux. That’s why enteric-coated capsules (like IBgard) are recommended-they release the oil in the intestine, not the stomach. If you get heartburn, switch to a branded enteric-coated version or reduce the dose. Not everyone reacts the same.
Can stress management really change my bowel habits?
Yes. Your gut and brain are connected by the vagus nerve. When you’re stressed, your gut slows down or speeds up unpredictably. CBT and breathing techniques help your brain stop overreacting to normal gut signals. Studies show this reduces pain and improves stool consistency-not just by making you feel calmer, but by changing how your body responds.
How long before I see results from the low FODMAP diet?
Most people notice improvement within 2-4 weeks. If you don’t see changes by week 6, you may need to check for other triggers-like lactose intolerance, caffeine, or fat intake. Don’t give up too soon, but don’t stay on elimination longer than 6 weeks without guidance.
Are there any new medications coming for IBS-Mixed?
Yes. Ibodutant, a new neurokinin-2 receptor antagonist, showed 45% improvement in IBS-M symptoms in phase 3 trials. It’s expected to be available by late 2025 or early 2026. Unlike older drugs, it targets both pain and bowel irregularity without worsening one symptom to fix the other. This could be a game-changer for IBS-M patients.


Ryan Pagan
January 29, 2026 at 16:28Man, this post is a godsend. I’ve been cycling between constipation and diarrhea for years and felt like I was going crazy. The part about antidepressants helping with gut nerves? Mind blown. I was on sertraline for anxiety and didn’t realize it was also calming my gut. Started tracking with Bowel Buddy and cut out garlic and onions-my flare-ups dropped by 60% in three weeks. No more canceling weekend plans. This isn’t just advice-it’s a lifeline.
DHARMAN CHELLANI
January 31, 2026 at 14:32fodmap is just a fad. eat meat and rice. problem solved. why overcomplicate?
Paul Adler
February 1, 2026 at 18:07While I appreciate the thoroughness of this breakdown, I have to respectfully note that the emphasis on pharmaceuticals might overshadow the foundational role of gut-brain axis regulation. The fact that CBT shows more consistent results than many medications suggests we’re still treating symptoms rather than root neurophysiological dysregulation. That said-kudos on the practicality. The tracking advice alone is worth a thousand blog posts.
Alex Flores Gomez
February 3, 2026 at 11:38low fodmap? pfft. i tried that and still got bloated. turns out its just the dairy. everyone overcomplicates things. just cut out milk. done. also, peppermint oil is for hippies. real men take imodium and move on.
Robin Keith
February 4, 2026 at 18:57Let us not forget, dear interweb wanderers, that the gut-this ancient, primordial, neurologically labyrinthine organ-is not merely a digestive tract, but a sentient echo of our emotional architecture; a living cathedral of neurotransmitters, microbial choirs, and autonomic symphonies that have, for millennia, whispered in the dark corners of our nervous systems… and yet, we reduce it to a spreadsheet of Bristol scores and loperamide doses? We are, in essence, trying to map the soul of a hurricane with a ruler. The low-FODMAP diet? A beautiful, temporary scaffolding. But the true healing? It lies in the quiet, the breath, the unspoken surrender to the rhythm of the body-not the control of it. I’ve wept in bathrooms, yes-but I’ve also wept in meditation, and in those tears, I found not relief… but communion.
Kristie Horst
February 4, 2026 at 22:46How charming. Someone actually wrote a comprehensive, evidence-based guide-and the first three replies are from people who think ‘just avoid dairy’ is a cure-all. Honestly, if you’re going to dismiss decades of clinical research because you read a blog post in 2017, maybe don’t comment? The low FODMAP diet isn’t about restriction-it’s about discovery. And yes, peppermint oil capsules are enteric-coated for a reason. If you’re getting heartburn, you’re using the wrong product. This isn’t witchcraft. It’s medicine. Please, for the love of all that is holy, consult a dietitian before you self-diagnose your colon.
Frank Declemij
February 6, 2026 at 00:51Psyllium husk works. 5g daily. No drama. No magic. Just fiber. I’ve been doing this for 18 months. No meds. No apps. Just consistency. The rest is noise.
paul walker
February 6, 2026 at 07:09OMG YES. I tried everything. Pills, diets, yoga, crystals (yes, really). The only thing that stuck was the tracking app + psyllium. I used to have 25 bad days a month. Now it’s like 5. Still not perfect, but I can travel again. Also, IBS-M is not your fault. You’re not weak. You’re not broken. Just… weirdly wired. And you’re not alone.
Sheryl Dhlamini
February 6, 2026 at 17:51I cried reading this. Not because it’s sad-but because for the first time, someone described my life exactly. The fear before every meal? The canceled plans? The meds that help one thing and wreck the other? I thought I was the only one. Thank you. I’m starting the low FODMAP diet tomorrow. And I’m buying IBgard. No more suffering in silence.
Andy Steenberge
February 6, 2026 at 19:48For anyone considering ibodutant: it’s promising, but don’t hold your breath. Phase 3 trials are great, but FDA approval takes 18–24 months minimum. Meanwhile, the tools here-psyllium, low FODMAP, CBT, and targeted loperamide/Miralax-are proven, accessible, and free from corporate hype. Also, if you’re using a generic peppermint oil capsule, stop. You’re not getting the enteric coating. IBgard, Fybogel, or similar-don’t cheap out on your gut health. And yes, antidepressants for IBS? Totally valid. It’s not depression-it’s neuromodulation. Your brain and gut are wired together. Treat both.
Keith Oliver
February 8, 2026 at 18:18Look, I’ve been doing this for 12 years. You think you’re special because you tracked your poop? Everyone’s done that. The real secret? Probiotics. Not the yogurt crap-like Visbiome or Seed. I’ve been on it for 8 months. My stools are regular. No meds. No dieting. Just good bugs. Also, stop obsessing over FODMAPs. Most of it’s placebo. Your gut just needs balance. And no, I don’t work for them. I just don’t like when people overcomplicate simple biology.
Ryan Pagan
February 10, 2026 at 09:16Actually, the Visbiome study you mentioned? It showed benefit in IBS-D, but not IBS-M. The same 2022 meta-analysis that looked at 17 probiotic strains found only two had any effect on mixed IBS-and one of them was L. plantarum 299v, which isn’t even in Visbiome. Just saying-don’t swap one fad for another. Psyllium and CBT? Those have Level 1 evidence. Probiotics? Still a mixed bag. Especially for IBS-M.