What Happens When a Prescription Drug Becomes Over-the-Counter?
Every year, a few medications make the leap from behind the pharmacy counter to the shelf next to pain relievers and cold medicine. This isn’t just a marketing move-it’s a carefully reviewed regulatory decision. When a drug switches from prescription (Rx) to over-the-counter (OTC), it means the FDA has determined that, for most people, it’s safe enough to use without a doctor’s order. But safety doesn’t mean risk-free. The same pill that helps someone manage a headache without a visit to the clinic can cause serious harm if used incorrectly.
The first big switch happened with ibuprofen. In 1984, it went from a prescription-only painkiller to a common OTC option. That change didn’t just make it cheaper-it made it easier to get. Within months, prices dropped from $30-$40 a month to $5-$10. Millions of people gained access. But it also meant more people were taking it without knowing if it was right for them.
Why Do Drugs Switch from Prescription to OTC?
The goal isn’t to cut corners-it’s to cut unnecessary visits. If a condition is easy to self-diagnose (like occasional heartburn, mild allergies, or minor aches), and the medicine has a wide safety margin, regulators consider moving it to OTC status. The FDA looks at three main things: Can people understand the label? Will they use it correctly? And is the risk low enough that skipping a doctor’s visit won’t cause more harm than good?
For example, omeprazole (Prilosec OTC) switched in 2003. It treats frequent heartburn, a common issue. Most people know when they have it. The drug is stable, doesn’t interact badly with many other medicines, and has clear dosing instructions. So, letting people buy it without a script made sense. But for drugs treating complex conditions-like high blood pressure, diabetes, or depression-switching isn’t even considered. Too many variables. Too much risk.
The Hidden Dangers: What Most People Don’t Realize
Here’s the problem: most people don’t treat OTC drugs like real medicine. They think, “It’s on the shelf, so it’s harmless.” That’s dangerous. Acetaminophen, the active ingredient in Tylenol, is the leading cause of acute liver failure in the U.S. Why? Because people take it with other cold medicines that also contain acetaminophen. They don’t realize they’re doubling up. One study found nearly half of consumers didn’t check the active ingredients before combining OTC products.
NSAIDs like ibuprofen and naproxen are another silent risk. Used short-term for a sprained ankle? Fine. Used daily for months because your back still hurts? That’s when things go wrong. Long-term use can lead to stomach ulcers, kidney damage, or even heart attacks-especially in older adults or people with high blood pressure. And if you’re on blood thinners? That’s a recipe for trouble. The FDA warns that mixing aspirin with warfarin can cause dangerous bleeding, yet many people still do it without asking a pharmacist.
Decongestants like pseudoephedrine are another trap. They’re great for a stuffy nose. But if you have high blood pressure or take certain antidepressants, they can spike your blood pressure to life-threatening levels. One pharmacist in Melbourne reported seeing three elderly patients in a single month with severe hypertension after starting OTC cold meds. None of them knew the warning was on the label.
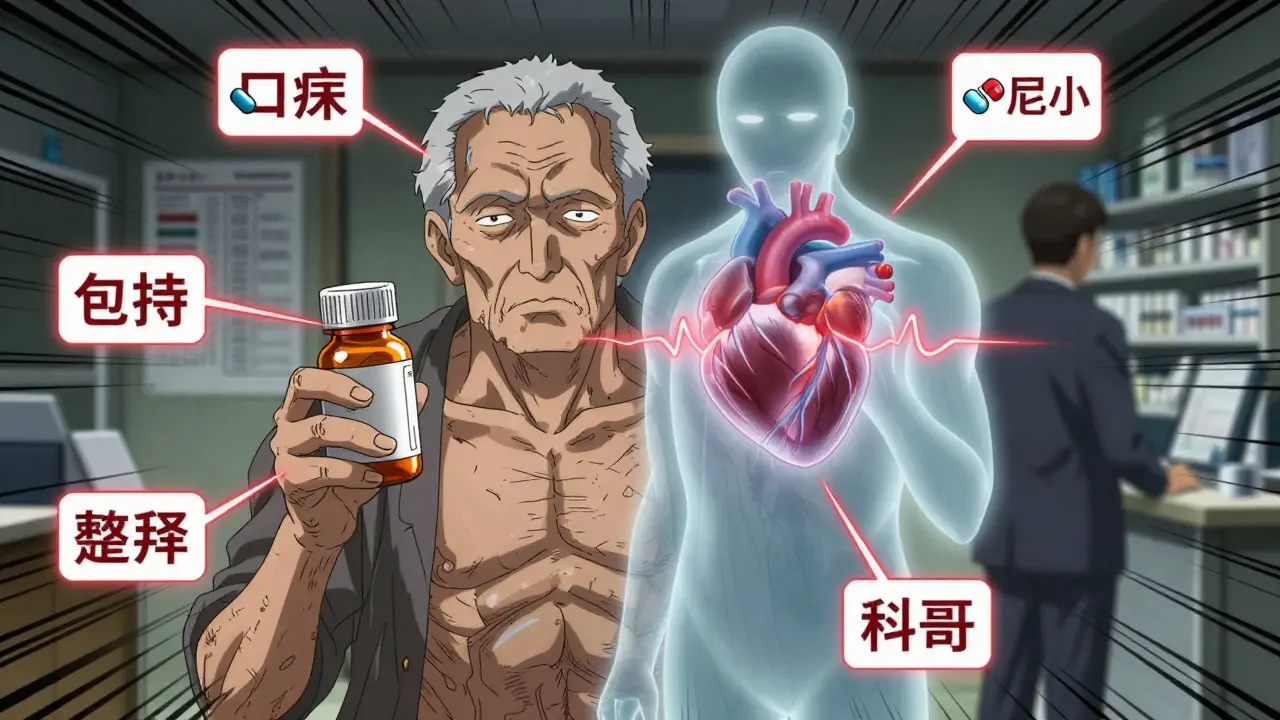
Who’s at the Highest Risk?
Not everyone is equally affected by OTC switches. Certain groups need extra caution:
- Older adults (65+): Their bodies process drugs slower. The American Geriatrics Society lists 30 OTC medications as risky for this group-like diphenhydramine (Benadryl), which can cause confusion, dizziness, and falls.
- People taking multiple medications: If you’re on five or more drugs, the chance of a bad interaction jumps. OTC meds add to that mix. One in four adults over 65 takes at least one OTC drug daily without telling their doctor.
- People with chronic conditions: Diabetes, kidney disease, liver problems, asthma, or heart disease all change how your body handles drugs. What’s safe for one person can be deadly for another.
- Children: Giving adult-strength OTC medicine to kids is still common. Even small overdoses of acetaminophen or cough syrups can lead to hospitalization.
And here’s the kicker: many people don’t tell their doctor they’re using OTC meds. They think it’s not “real” medicine. But your doctor needs to know everything you’re taking-even the stuff you bought without a script.
How to Use OTC Medicines Safely
Just because you don’t need a prescription doesn’t mean you shouldn’t be smart about it. Here’s how to stay safe:
- Read the Drug Facts label. It’s not filler. It’s your safety guide. Look at the active ingredients first. If two products have the same one, don’t take them together.
- Check for warnings. Does the label say “Do not use if you have high blood pressure”? If you do, skip it. Even if you’ve used it before, conditions change. Your body changes.
- Ask your pharmacist. You don’t need a prescription to talk to them. Pharmacists are trained to spot interactions. Tell them what prescriptions you’re on, even if you think it’s unrelated. They’ve seen the mistakes before.
- Don’t use it longer than the label says. If your headache lasts more than 10 days, your cold drags on for three weeks, or your heartburn won’t quit-see a doctor. OTC meds are for short-term relief, not long-term fixes.
- Use one pharmacy. If you get all your meds from the same place, the pharmacist can track what you’re taking and flag potential conflicts.
There’s a reason the FDA updated the Drug Facts label in 2022: bigger fonts, clearer warnings, simpler language. But if you’re not reading it, the design doesn’t matter.

What’s Changing Now?
The future of OTC safety is digital. Some pharmacies are testing QR codes on OTC packaging that link to video instructions, interaction checkers, and updated warnings. Walmart started this pilot in 2023. It’s still early, but the idea is simple: if you scan the code, you get personalized info based on your age, meds, and conditions.
Regulators are also pushing for better post-market tracking. Instead of waiting for people to report side effects, they’re looking at electronic health records and pharmacy data to spot patterns faster. If 200 people in a region start going to ERs with liver issues after using a new OTC pain reliever, that’s a red flag.
But technology won’t fix the real problem: lack of awareness. A study in Bangalore found that 77% of patients didn’t know the contraindications for their OTC drugs. And nearly 85% believed their pharmacist gave them full advice-even when the pharmacist didn’t ask about their other meds or health history.
The Bottom Line
OTC switches are a win for convenience and cost. But they’re not a win for ignorance. The same drug that helps you get through a busy week can quietly damage your liver, kidneys, or heart if used carelessly. The key isn’t to avoid OTC meds-it’s to treat them like the powerful medicines they are.
Ask yourself: Do I really need this? Am I sure it’s safe with my other meds? Have I checked the label? If the answer to any of those is “I’m not sure,” then talk to someone who knows-your pharmacist, your doctor, or even a trusted health website. Don’t guess. Don’t assume. And don’t forget: just because it’s on the shelf doesn’t mean it’s harmless.
Are OTC medications safer than prescription drugs?
No, OTC medications aren’t inherently safer-they’re just approved for use without a doctor’s supervision under specific conditions. Many OTC drugs, like NSAIDs and acetaminophen, carry serious risks if misused. The difference isn’t in safety, but in oversight. Prescription drugs come with a doctor’s guidance; OTC drugs rely on the user reading labels and making smart choices.
Can I take OTC painkillers if I’m on blood pressure medicine?
It depends. NSAIDs like ibuprofen and naproxen can raise blood pressure and reduce the effectiveness of some blood pressure meds. Acetaminophen is usually safer for people with hypertension, but it’s not risk-free-especially if you drink alcohol or have liver issues. Always check the label and ask your pharmacist before combining OTC pain relievers with prescription blood pressure drugs.
Why do OTC labels warn against using decongestants with antidepressants?
Decongestants like pseudoephedrine can cause dangerous spikes in blood pressure and heart rate when mixed with certain antidepressants, especially MAOIs or tricyclics. This interaction can lead to stroke, heart rhythm problems, or even death. These warnings exist because the risk is real and documented. Even if you’ve taken both before without issue, your body’s response can change over time.
Is it safe to give OTC cold medicine to my child?
For children under 6, the FDA advises against using OTC cough and cold medicines. They’re not proven to work and can cause serious side effects like rapid heart rate, seizures, or even death. For older kids, always use the child-specific dose and avoid adult formulas. Never give aspirin to children-it can cause Reye’s syndrome, a rare but life-threatening condition.
What should I do if I accidentally take too much of an OTC drug?
If you suspect an overdose-especially with acetaminophen, NSAIDs, or sleep aids-call poison control immediately (1-800-222-1222 in the U.S.) or go to the nearest ER. Don’t wait for symptoms. Acetaminophen overdose can cause liver damage before you feel sick. Bring the medicine bottle with you so medical staff know exactly what was taken.
Do pharmacists always check for drug interactions when I buy OTC meds?
Not always. While most pharmacists will ask if you’re on other medications, many don’t proactively review your full list unless you bring it up. A 2022 survey found only 32% of people consistently read OTC labels, and many pharmacists don’t ask about existing conditions like high blood pressure or kidney disease. Don’t assume they know-tell them. Bring a list of everything you take, including supplements.




Katharine Meiler
February 4, 2026 at 01:20The FDA's OTC switch criteria are rigorously evidence-based, but real-world adherence is a different beast. The label readability improvements post-2022? Great. But cognitive load still overwhelms elderly users. I've reviewed pharmacovigilance data from Kaiser Permanente - polypharmacy patients on 5+ meds are 3.7x more likely to overdose on OTC acetaminophen when they don't disclose OTC use. We need mandatory pharmacist counseling at point-of-sale for high-risk categories, not just 'ask if you have questions.' This isn't convenience - it's a public health blind spot.
Danielle Vila
February 4, 2026 at 18:12Let’s be real - Big Pharma orchestrated this whole OTC switch circus to turn prescription profits into repeat retail sales. They don’t care if you kill your liver - they care about your monthly $12 ibuprofen habit. And don’t get me started on the QR code ‘solution.’ That’s just surveillance capitalism in a pill bottle. Your scan data gets sold to insurers who jack up your premiums because you ‘self-medicated.’ The FDA? A revolving door of ex-pharma execs. Wake up. They’re not protecting you - they’re monetizing your ignorance.
Thorben Westerhuys
February 4, 2026 at 18:47I just... I just took two Advil for my back... and then I read this... and now I’m terrified... I didn’t even know... I’ve been taking it for months... I have high blood pressure... I didn’t think... Oh my god... I need to call my pharmacist... right now... I feel sick... I think I’m going to be sick...
Laissa Peixoto
February 6, 2026 at 02:20What’s fascinating here isn’t just the pharmacology - it’s the epistemological shift. OTC drugs represent a transfer of medical authority from clinician to consumer, but without adequate epistemic infrastructure. We’ve outsourced risk assessment to a 12-point label written at a 7th-grade reading level, while the average American’s health literacy hovers around 4th grade. The solution isn’t more warnings - it’s re-embedding clinical reasoning into everyday decision-making. Maybe community health liaisons? Or AI-driven label interpreters? The system isn’t broken - it’s profoundly misaligned.
Lana Younis
February 6, 2026 at 09:57Y’all need to chill. I’m 68, on 7 meds, and I’ve been using OTC stuff for decades. I read the label. I check with my pharmacist. I use one pharmacy. It’s not that hard. I’ve seen people panic over labels like they’re ancient scrolls. The real issue? People don’t talk to their care team. I told my pharmacist I was taking NyQuil with my blood pressure med - she laughed and said ‘that’s why we have you on file.’ Just be a little proactive. Don’t turn every pill into a crisis. Also - QR codes? YES. My grandkid scanned mine and it told me to avoid it with my Zoloft. Saved my life. Tech ain’t evil - lazy thinking is.
Samantha Beye
February 6, 2026 at 23:41Reading this made me think of my mom. She took ibuprofen daily for her arthritis. Never told her doctor. Thought it was ‘just aspirin.’ Last year, she had a GI bleed. She’s fine now, but it changed everything. I started sending her weekly ‘OTC check-ins’ - just a text: ‘Did you check your labels this week?’ She rolls her eyes, but she does it. Small habits matter. You don’t need a PhD to stay safe - just a little attention. And a reminder. I’m proud of her.
Rene Krikhaar
February 8, 2026 at 05:53I work at a community pharmacy and I see this every day. People come in for cold medicine and never say they’re on warfarin or lisinopril. I ask. They say oh I forgot. I remind them. I’m not mad. I get it. Life’s busy. But if you don’t tell us, we can’t help. We’re not mind readers. We’re just trying to keep you from ending up in the ER. So next time you grab something off the shelf - pause. Look at the label. Tell us what you’re on. We’ve got your back.
Lisa Scott
February 10, 2026 at 05:52Let’s cut the corporate PR fluff. The OTC switch is a profit-maximization strategy disguised as consumer empowerment. Acetaminophen’s hepatotoxicity is a known, documented risk since the 70s. Why wasn’t it pulled? Because the market is too lucrative. The FDA’s ‘safety margin’ is a statistical fiction built on low-risk cohorts. Real-world usage? It’s a minefield. And now they’re pushing QR codes? That’s not safety - it’s data harvesting. They want your health records, your habits, your patterns. This isn’t healthcare. It’s surveillance capitalism with a Band-Aid.
Dina Santorelli
February 11, 2026 at 15:47Ugh. Another ‘read the label’ lecture. That’s like telling a diabetic to ‘just eat less sugar.’ The labels are written by lawyers, not doctors. And who has time? I’m working two jobs, raising kids, and my back hurts. I don’t have a PhD in pharmacology. The system is designed to fail people like me. And don’t even get me started on the ‘ask your pharmacist’ nonsense - they’re overworked, underpaid, and don’t even have time to look at your full med list. This whole thing is a scam. We’re being sold a false sense of safety while the real dangers multiply.
Arjun Paul
February 12, 2026 at 08:22India has been dealing with OTC misuse for decades. In rural areas, people buy antibiotics like candy. No regulation. No counseling. The result? Antibiotic resistance is out of control. The U.S. thinks it’s smarter? Think again. The same mindset exists - ‘if it’s on the shelf, it’s harmless.’ We need mandatory public health campaigns. Not QR codes. Not labels. Real education. From school. From TV. From community centers. Technology is not the solution - awareness is.
one hamzah
February 14, 2026 at 01:00OMG this is so true!! 🙌 I’m from Mumbai and we’ve got pharmacies on every corner - no prescriptions needed for anything! I used to take OTC painkillers for my migraines… then I found out they were raising my BP 😱 Now I always ask the pharmacist - they’re actually super helpful here! 🤝 And I scan QR codes now - it tells me about interactions in Hindi too!! 📱❤️ We need more of this in the US - not just tech, but culture. OTC meds = power. Use them wisely, not blindly. #PharmacistLove #ReadTheLabel