When you hear Crohn’s disease and ulcerative colitis, they might sound like the same thing - both cause stomach pain, diarrhea, and fatigue. But they’re not. They’re two different diseases that fall under the same umbrella: inflammatory bowel disease (IBD). And knowing the difference isn’t just academic - it changes everything about how you’re treated, what complications you might face, and even what your daily life looks like.
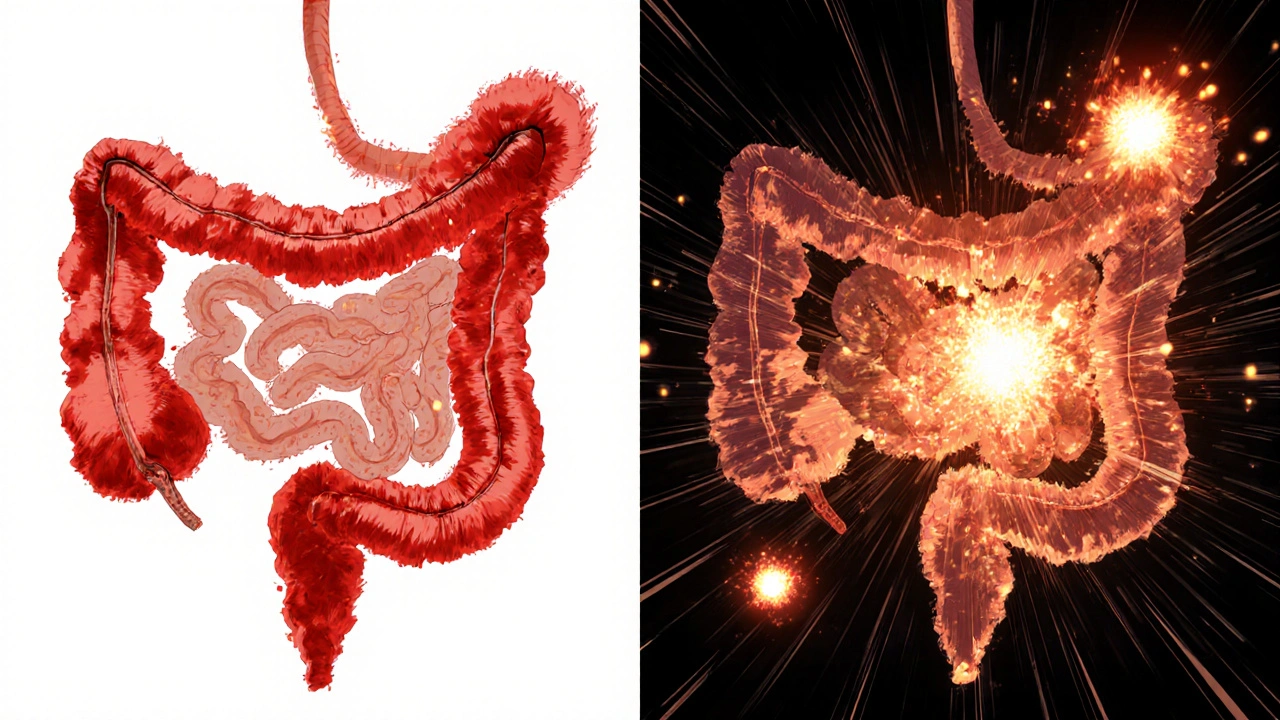
Where the Inflammation Happens
- Ulcerative colitis only affects the colon and rectum - the last part of your digestive tract. The inflammation starts at the rectum and moves upward in a continuous line. There are no gaps. It’s like a burn that spreads evenly along a straight line.
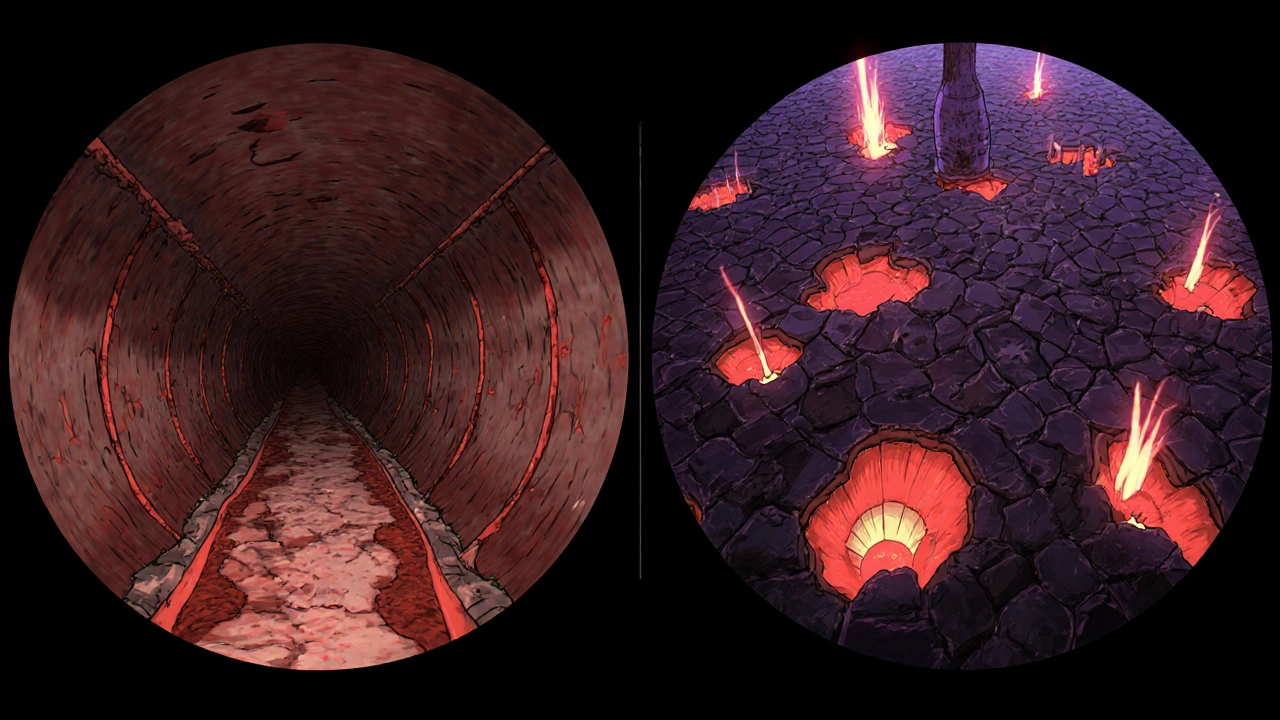
- Crohn’s disease can show up anywhere from your mouth to your anus. Most often, it hits the end of the small intestine (ileum) and the beginning of the colon. But it can pop up in patches - healthy tissue between inflamed areas. These are called “skip lesions.” It’s not a straight line. It’s more like scattered fire spots.
This difference isn’t just about location - it affects what symptoms you feel. If you have ulcerative colitis, you’re more likely to feel urgent, frequent bowel movements with bright red blood. If you have Crohn’s, you might feel pain deeper in your belly, or even near your anus, and you might have trouble absorbing nutrients because your small intestine is involved.
How Deep the Damage Goes
Ulcerative colitis stays shallow. It only eats away at the inner lining of the colon - the mucosa and maybe the layer just below it. That’s why bleeding is so common. The surface is literally ulcerated.
Crohn’s disease goes deeper. It doesn’t stop at the surface. It burns through all layers of the bowel wall - all the way to the outer membrane. This is called transmural inflammation. And that’s why Crohn’s leads to complications that ulcerative colitis rarely does: strictures (narrowing from scar tissue), fistulas (abnormal tunnels between organs), and abscesses. About one in three people with Crohn’s will develop a stricture over their lifetime. One in four will get a fistula. Those complications almost never happen in ulcerative colitis.
What Shows Up on Tests
Doctors use colonoscopies to look inside your colon. In ulcerative colitis, they see a uniform, red, raw-looking lining with tiny ulcers and sometimes pseudopolyps - raised bumps from healing tissue. It’s consistent from the rectum up.
In Crohn’s, the view is patchy. They see cobblestoning - a bumpy, uneven surface from deep ulcers separated by normal tissue. They might also spot fistulas or thickened bowel walls. If the colon looks normal but you still have symptoms, doctors might order a capsule endoscopy (a pill-sized camera you swallow) to check your small intestine. That’s where Crohn’s often hides.
Blood and stool tests help too. A stool test for calprotectin (a protein that signals inflammation) is usually higher in ulcerative colitis. A blood test for pANCA antibodies is positive in 60-70% of ulcerative colitis patients but only 10-15% of Crohn’s patients. These aren’t perfect, but they’re clues that help put the puzzle together.
Complications That Set Them Apart
Ulcerative colitis has one scary complication: toxic megacolon. That’s when the colon swells dangerously and can rupture. It happens in about 5% of severe flare-ups. It’s rare in Crohn’s.
Crohn’s has its own nightmares: fistulas. These are tunnels that form between your intestine and other organs - maybe your bladder, skin, or vagina. They can leak pus or stool. About 25% of people with Crohn’s will develop them. You won’t see this in ulcerative colitis.
Both can cause joint pain, skin rashes, or eye inflammation - but one condition has a special link to liver disease. Primary sclerosing cholangitis (PSC), a rare liver condition that scars the bile ducts, affects 3-7% of ulcerative colitis patients. In Crohn’s, it’s less than 1%. If you have PSC, your doctor will assume you have ulcerative colitis until proven otherwise.
Treatment Differences
Because ulcerative colitis only affects the colon, you can treat it with medications that go right to the source. Suppositories and enemas with 5-ASA drugs (like mesalamine) work well for mild to moderate cases. They deliver the medicine directly to the inflamed area. About 60-80% of patients respond.
Crohn’s needs systemic treatment. Pills or injections that work throughout your whole body. Immunosuppressants like azathioprine or biologics like infliximab and adalimumab are common. These drugs target the immune system’s overreaction. In clinical trials, about 30-40% of Crohn’s patients go into remission with anti-TNF drugs after a year. For ulcerative colitis, the same drugs work - but less often, around 20-30%.
Here’s the biggest difference: surgery.
If you have ulcerative colitis, removing your entire colon and rectum - a total proctocolectomy - is a cure. Many people get an ileal pouch built from the small intestine and attached to the anus. They can still pass stool normally. About 10-15% of ulcerative colitis patients end up needing this surgery within 10 years.
Crohn’s doesn’t work that way. Even if you remove the diseased part of the intestine, the disease comes back - often right next to the surgical site. Half of Crohn’s patients need another surgery within 10 years. Surgery helps relieve symptoms, but it’s not a cure.

What Patients Actually Experience
Real people report real differences. On IBD forums, ulcerative colitis patients say they live with constant urgency - the sudden, uncontrollable need to go. About 87% report this, compared to 68% of Crohn’s patients. Rectal bleeding? 75% of UC patients see it. Only 35% of Crohn’s patients do.
Crohn’s patients talk more about nutrition. Because their small intestine is often affected, they struggle with absorbing vitamins and calories. Weight loss and fatigue are common. One in three says they’ve lost significant weight because their body couldn’t absorb food properly.
Triggers differ too. On Reddit’s IBD community, stress is the top trigger for ulcerative colitis flare-ups. For Crohn’s, it’s food. Dairy and high-fiber meals like raw veggies or whole grains come up again and again.
When It’s Not Clear - Indeterminate Colitis
Even with all these tools, about 10-15% of cases can’t be clearly labeled at first. Doctors call this “indeterminate colitis.” You might have features of both. That’s okay. It doesn’t mean something’s wrong with the diagnosis - it means the disease is still revealing itself.
Studies show that over five years, about 12% of people initially diagnosed with ulcerative colitis end up being reclassified as Crohn’s. Why? Because they develop fistulas, skip lesions, or deep ulcers - signs that only Crohn’s shows. That’s why doctors keep monitoring. Your diagnosis might change - and that’s normal.
What’s Next for Treatment
New drugs are coming. For ulcerative colitis, etrolizumab is in late-stage trials. For Crohn’s, mirikizumab showed strong results in 2023 and could be approved by late 2024. Both target different parts of the immune system than older biologics.
Fecal microbiota transplants (FMT) - basically, a poop transplant - have shown promise. In ulcerative colitis, FMT led to remission in 32% of patients in one trial. For Crohn’s, it was only 22%. That tells us the gut bacteria play different roles in each disease.
Costs reflect the complexity. On average, severe Crohn’s costs nearly $40,000 a year in medical care. Severe ulcerative colitis runs about $38,000. But mild Crohn’s is more expensive than mild UC - because it’s harder to control.
And the numbers are rising. IBD affects about 0.5% of people in the U.S. and Europe. In countries that were recently industrialized, cases have jumped 50% in the last 20 years. Why? Probably a mix of diet, hygiene, antibiotics, and environmental changes - but no one knows for sure yet.
What matters now is this: if you or someone you know has IBD, knowing whether it’s Crohn’s or ulcerative colitis isn’t just about labels. It’s about choosing the right treatment, preparing for possible complications, and understanding what your body is really doing.
Can you have both Crohn’s disease and ulcerative colitis at the same time?
No, you can’t have both at the same time. They’re two separate diseases. But sometimes, early symptoms look so similar that doctors can’t tell which one it is right away. That’s called indeterminate colitis. Over time, as symptoms or test results change, the diagnosis usually becomes clear - and you’re reclassified as having one or the other.
Is one disease worse than the other?
Neither is inherently “worse.” They just cause different problems. Ulcerative colitis can lead to life-threatening complications like toxic megacolon. Crohn’s causes more long-term structural damage - strictures, fistulas, and recurring need for surgery. Both can be disabling if not managed. The severity depends on the individual, not the label.
Can diet cure Crohn’s or ulcerative colitis?
No diet can cure either disease. But diet can help manage symptoms. People with Crohn’s often find that avoiding high-fiber or dairy foods reduces flare-ups. Those with ulcerative colitis may benefit from low-residue diets during flares. Some people report success with specific plans like the Specific Carbohydrate Diet, but there’s no one-size-fits-all solution. Always work with a dietitian who knows IBD.
Do I need surgery if I have ulcerative colitis?
Not everyone does. Many people control their symptoms with medication for years. But if medications stop working, or if you develop precancerous changes in the colon, surgery becomes the best option. A total removal of the colon and rectum is the only cure for ulcerative colitis - and many people who have it report better quality of life afterward.
Can IBD turn into cancer?
Yes, long-standing ulcerative colitis increases the risk of colon cancer - especially if the whole colon is affected for more than 8-10 years. That’s why regular colonoscopies with biopsies are critical. Crohn’s disease also raises cancer risk, but mainly in the small intestine or areas with chronic inflammation. Surveillance and good control of inflammation reduce this risk significantly.


steffi walsh
November 18, 2025 at 18:35Just read this and cried a little 😭 I was diagnosed with UC last year and this broke down everything I’ve been too scared to ask about. Thank you for writing this like someone actually cares.
Leilani O'Neill
November 20, 2025 at 06:36Ugh, another one of those ‘IBD is just a fancy word for bad digestion’ articles. People need to stop romanticizing chronic illness like it’s a wellness trend. This isn’t a Pinterest board.
Riohlo (Or Rio) Marie
November 20, 2025 at 10:55Let’s be real - this is the most coherent breakdown of IBD I’ve seen since my gastroenterologist tried explaining it over a 20-minute coffee break while I was mid-flare. The ‘skip lesions = scattered fire spots’ analogy? Chef’s kiss. 🫶 The fact that you mentioned pANCA and calprotectin without sounding like a textbook? Revolutionary. I’m sending this to my entire family. They still think I’m ‘just stressed.’
Conor McNamara
November 21, 2025 at 10:03did u know the gov is using ibd to track ppl through their poop? they put microchips in the meds now. i read it on a forum. my doctor wont talk about it. i think theyre watching me.
Kristi Joy
November 22, 2025 at 10:44This is such a gift to anyone newly diagnosed. I wish I’d had this when I was first told I had Crohn’s - I felt so alone. You made the science feel human. Keep doing this work.
Hal Nicholas
November 22, 2025 at 20:22Everyone’s acting like this is groundbreaking. I’ve been on Reddit for 12 years. We’ve known all this. The real issue? Insurance won’t cover the biologics unless you’ve failed 7 other drugs first. And no one talks about that.
Louie Amour
November 24, 2025 at 08:19Wow. This is basically a 2000-word ad for Big Pharma. You mention biologics like they’re magic pills. Ever heard of the fact that 60% of people on infliximab lose response within a year? Or that FMT is still experimental? You’re giving false hope to vulnerable people.
Kristina Williams
November 25, 2025 at 10:58So basically, if you have UC you bleed a lot and if you have Crohn’s you get fat and sick? That’s it? I thought it was more complicated. My cousin says she’s got both. Is that even possible? I’m confused now.
Shilpi Tiwari
November 26, 2025 at 04:05From a clinical immunology standpoint, the differential expression of IL-23/Th17 axis in Crohn’s versus the epithelial barrier dysfunction in UC is the key molecular divergence. The pANCA positivity in UC correlates with MPO-specific autoantibodies, while ASCA in Crohn’s targets yeast mannans - both are serologic biomarkers with >85% specificity in meta-analyses. The microbiome dysbiosis profiles also differ significantly, with Faecalibacterium prausnitzii depletion being more pronounced in Crohn’s.
Christine Eslinger
November 28, 2025 at 02:48I’ve been living with Crohn’s for 17 years. Surgery didn’t cure me - but it gave me back my life. I used to be afraid of eating anything. Now I can have a taco. I know it sounds small. But it’s everything. This post? It’s the kind of thing I wish I’d had when I was 22, scared, and alone in a hospital bed. Thank you for saying it like it is - no sugar, no fluff. Just truth.
Denny Sucipto
November 29, 2025 at 02:23Man, I’ve been through all this. The fistula that leaked for 11 months. The 3 a.m. ER visits. The way your friends slowly stop asking if you want to go out. This isn’t just medical stuff - it’s a whole new way of living. And yeah, sometimes you just want someone to say ‘yeah, that sucks’ without trying to fix it. You did that. I appreciate it.