For decades, diagnosing and tracking cancer meant drilling into the body-cutting, scraping, and pulling out tissue. It was painful. Risky. And often too late. Today, a simple blood draw is doing what biopsies could never do: showing doctors what’s happening inside a tumor in real time, without a single incision. This isn’t science fiction. It’s liquid biopsy, and it’s already changing how cancer is managed.
What Exactly Is Liquid Biopsy?
Liquid biopsy isn’t a single test. It’s a whole new way of looking at cancer by analyzing tiny pieces of it floating in your blood. The most important piece? Circulating tumor DNA, or ctDNA. When cancer cells die, they break apart and spill fragments of their DNA into the bloodstream. These fragments carry the same mutations that drive the tumor. By catching and decoding them, doctors get a molecular snapshot of the cancer-without touching the tumor itself.It’s not just DNA. Liquid biopsy can also pick up tumor cells floating in the blood, RNA, and even tiny bubbles released by tumors called extracellular vesicles. But ctDNA is the star. It’s stable, abundant in many cancers, and reflects the tumor’s genetic changes as they happen.
Why It Beats Traditional Biopsies
A tissue biopsy is like taking one photo of a painting. If the brushstrokes vary across the canvas, you miss half the story. Tumors aren’t uniform. One part might have a mutation that makes it resistant to treatment. Another might be growing fast. A single needle stick can’t capture that.Liquid biopsy sees the whole picture. In metastatic cancers, up to 30% of important mutations are missed by tissue biopsies because they’re only sampling one spot. Liquid biopsy pulls DNA from every part of the tumor, everywhere it’s spread. That’s why, in advanced lung cancer, guidelines now say: if tissue isn’t enough, use a blood test first.
And then there’s the risk. Tissue biopsies for lung, liver, or pancreatic tumors can cause bleeding, infection, or even collapsed lungs. About 1-5% of patients face serious complications. Liquid biopsy? A needle in your arm. No anesthesia. No recovery time. You can do it every few weeks.
How It’s Used in Real-World Cancer Care
This isn’t just theory. It’s in use right now in major cancer centers.After surgery for colon or breast cancer, doctors want to know: did they get it all? Imaging can’t see microscopic leftovers. But ctDNA can. Studies show liquid biopsy detects minimal residual disease-tiny traces of cancer-up to 11 months before a scan shows anything. That’s huge. It means treatment can start earlier, when it’s most effective.
During treatment, ctDNA levels drop as the tumor shrinks. If they stay high or start rising again, it’s a red flag. Often, this happens months before a patient feels worse or a scan shows growth. In one study, doctors spotted resistance mutations in EGFR-positive lung cancer patients six months before imaging confirmed progression. That’s enough time to switch drugs before the cancer runs wild.
And it’s not just for tracking. Liquid biopsy is helping pick the right drug from the start. In non-small cell lung cancer, about 92% of cases where tissue was too small or damaged still yielded a clear targetable mutation from blood. That’s life-changing. No more waiting weeks for tissue results. No more missing out on targeted therapy because the biopsy failed.
The Limits: When It Doesn’t Work
It’s not magic. Liquid biopsy has blind spots.Early-stage cancers shed very little DNA. For stage I tumors, detection rates are only 50-70%. That’s why it’s not yet used for general screening in healthy people. But for high-risk groups-like those with strong family histories or genetic syndromes-it’s becoming a powerful tool.
Some cancers barely leak DNA. Brain tumors, slow-growing prostate cancers, and certain blood cancers often produce too little ctDNA to detect reliably. Detection rates can fall below 40%. In these cases, tissue biopsy still wins.
Then there’s noise. Not every mutated DNA fragment in your blood comes from cancer. As we age, our blood cells can develop harmless mutations too-a phenomenon called clonal hematopoiesis. It affects 10-15% of people over 65. If you don’t know how to tell the difference, you might think a healthy person has cancer. That’s why labs now compare ctDNA results with white blood cell DNA to filter out false signals.
And sometimes, the test finds a mutation no one knows how to treat. About 15-20% of reports show variants of unknown significance. That creates anxiety without clear answers.
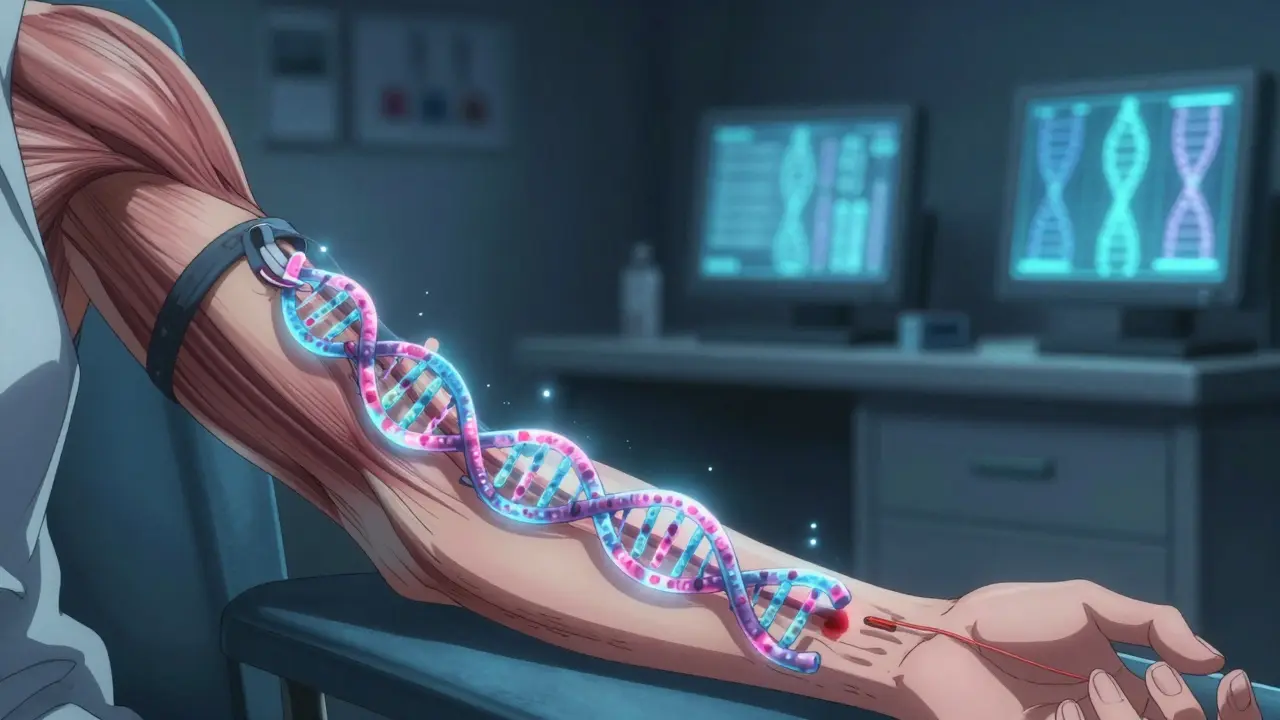
How the Test Is Done
It starts with a standard blood draw. Two tubes. That’s it.The blood is spun to separate plasma-the liquid part-where ctDNA hides. Then, labs use one of two main approaches:
- Tumor-informed testing: First, the original tumor tissue is sequenced to find its unique mutations. Then, the blood test looks only for those exact changes. It’s precise but takes time and needs tissue.
- Tumor-agnostic testing: The blood is scanned for hundreds of known cancer mutations at once, no tissue needed. It’s faster, broader, and ideal when tissue isn’t available.
Technologies vary. Digital droplet PCR can spot one mutant DNA molecule in 10,000 normal ones. Next-generation sequencing looks at thousands of genes at once. Newer methods, like nanopore sequencing, even analyze the size and shape of DNA fragments-something tumors do differently than healthy cells. Combine that with methylation patterns (chemical tags on DNA that change in cancer), and sensitivity jumps 20-30%.

Who’s Using It-and Who Isn’t
In top cancer centers like MD Anderson, liquid biopsy is routine. About 35-40% of phase I clinical trials now use ctDNA as a biomarker. Sixty to seventy percent of oncology departments in academic hospitals offer it.But in community clinics? Only 25-30% do. Why? Cost. A single test can run $1,000-$2,500. Insurance doesn’t always cover it unless it’s for a specific approved use-like EGFR testing in lung cancer. And interpretation isn’t simple. Not every doctor knows how to read the results or what to do with them.
Regulatory approval is catching up. The FDA has approved 12 liquid biopsy tests since 2020. Guardant360 CDx and FoundationOne Liquid CDx are now standard companion diagnostics for matching patients to targeted therapies.
ASCO updated its 2023 guidelines to say: for advanced non-small cell lung cancer, if tissue isn’t available, use liquid biopsy for initial testing. That’s a big deal. It means this isn’t experimental anymore. It’s part of the standard of care.
The Future: Smarter, Earlier, Broader
The next five years will change everything.Researchers are combining ctDNA with methylation patterns, fragment size analysis, and even immune signals in the blood. Multi-analyte tests are already hitting 95% sensitivity for early-stage detection in trials. That could mean screening for multiple cancers with one blood test-no colonoscopies, no mammograms, no CT scans.
Artificial intelligence is being trained to spot cancer patterns in DNA fragments. At MD Anderson, AI models analyzing ctDNA fragmentation are improving accuracy by 15-20%. Imagine a test that doesn’t just say “cancer,” but tells you where it started, how aggressive it is, and what it’s likely to do next.
And cost? It’s falling fast. As production scales and automation improves, tests could drop below $500 in the next few years. That’s when community clinics will catch up.
Experts predict liquid biopsy will become the standard for monitoring cancer within five to seven years. It could cut unnecessary scans by 20-25%, reduce invasive procedures, and help patients live longer with better quality of life.
What This Means for You
If you or someone you know is undergoing cancer treatment, ask: Can we use liquid biopsy to track this? It’s not for every cancer, but for many-especially lung, colorectal, breast, and melanoma-it’s already a game-changer.It’s not about replacing tissue biopsies entirely. It’s about giving doctors a continuous stream of information instead of one blurry snapshot. It’s about catching resistance before it spreads. It’s about knowing if the treatment is working before you feel sick.
This isn’t the future. It’s now. And it’s quieter, safer, and smarter than anything we had before.


Sean Feng
January 11, 2026 at 00:25This is wild. Just a blood draw and they know if the cancer is growing? No more scary needle biopsies? I’m sold.
Priscilla Kraft
January 11, 2026 at 04:14This is honestly one of the most hopeful advances in oncology I’ve seen in years. 🙌 The fact that we can catch recurrence months before scans is life-changing. I hope this becomes standard everywhere soon. Also, the part about filtering out clonal hematopoiesis? Genius. 👏
Jason Shriner
January 11, 2026 at 10:03so like… we’re just gonna start pulling dna outta blood and calling it a day? no one’s worried this is just fancy fortune telling? i mean, what if the machine says ‘cancer’ but you’re just old and your blood cells are having a midlife crisis? 🤔
Vincent Clarizio
January 11, 2026 at 20:58Let’s not pretend this is some revolutionary miracle-it’s a tool, not a savior. We’ve been told ‘the future is here’ since the 80s with PET scans and monoclonal antibodies. Liquid biopsy? It’s just the latest flavor of molecular snake oil wrapped in venture capital jargon. Sure, it works in controlled trials with elite labs and $3,000 machines-but tell that to the guy in rural Alabama whose insurance won’t cover it because ‘it’s not medically necessary’ until he’s stage IV. And don’t even get me started on VUS-variants of unknown significance. That’s not science, that’s anxiety laundering. You give someone a 15-page report full of cryptic mutations and say ‘we don’t know what this means’ and then wonder why people are terrified? Welcome to 21st-century medicine: more data, less clarity, and a whole lot of billing codes.
Sam Davies
January 12, 2026 at 11:54Cost is the real issue here. £2k per test? For what? A fancy blood test that sometimes says ‘maybe’? In the UK, we’ve got NICE to contend with-they’d laugh this out of the room unless it saved 10% more lives and cost less than a decent pint of IPA. Also, ‘tumor-agnostic’ sounds like a marketing term invented by someone who thinks ‘agnostic’ means ‘magic’.
Christian Basel
January 12, 2026 at 14:30The analytical sensitivity of ddPCR vs NGS is non-trivial. ctDNA fraction thresholds vary by tumor type-epithelial vs hematologic shedding kinetics are fundamentally different. Also, the limit of detection for low-VAF variants is still constrained by sequencing depth and error rates. Most community labs don’t have the bioinformatic pipelines to handle methylation deconvolution or fragmentomics. This isn’t plug-and-play.
Adewumi Gbotemi
January 14, 2026 at 06:00Very nice. In Nigeria, we still struggle to get basic scans. But if this can be made cheap and simple, it could save so many lives. Hope someone makes it affordable for the world, not just rich countries.
Matthew Miller
January 14, 2026 at 19:09Everyone’s acting like this is a breakthrough. Newsflash: it’s not. We’ve had ctDNA detection since 2012. What changed? Nothing. The same companies are just repackaging old tech with new AI buzzwords. And now they want you to pay $2,500 for a test that gives you false positives because some old guy’s white blood cells mutated? That’s not medicine, that’s a scam dressed in a lab coat.
Priya Patel
January 15, 2026 at 17:56Okay but imagine if we could screen for 5 cancers with one blood test and no prep? No colonoscopy prep? No mammogram squeeze? I’d get it every year. This feels like the future I’ve been waiting for 🥹
Jennifer Littler
January 17, 2026 at 01:20Fragmentomics + methylation profiling is where the real predictive power lies. The current assays are still too reliant on mutation burden. But when you layer in nucleosome positioning patterns and cfDNA size distributions, you get a biological signature that’s far more specific than SNV detection alone. Still, validation across diverse cohorts remains a bottleneck.
Alfred Schmidt
January 17, 2026 at 10:11Wait-so we’re just going to trust a blood test over a biopsy? What if it’s wrong? What if it misses something? What if it gives you a false sense of security? This is reckless. People are going to die because they skipped the ‘real’ test because some tech bro said ‘it’s just a blood draw.’ And then when the tumor’s in their liver, they’ll blame the doctor-but the doctor was just following the algorithm! This is dangerous.
Alex Smith
January 17, 2026 at 19:13Hey, just a heads-up-this tech isn’t just for advanced cancer. I’ve seen it used in high-risk BRCA+ patients to monitor for recurrence after prophylactic surgery. It’s not perfect, but it’s the best we’ve got. And yes, the cost sucks-but if we push for insurance reform and public funding, we can make this accessible. This isn’t sci-fi. It’s science. And it’s helping real people right now.
Roshan Joy
January 18, 2026 at 18:34Very cool! In India, we don’t have access to this yet, but I hope it comes soon. Maybe one day, even small clinics can use it. I’ve seen too many people lose time waiting for biopsy results. This could help so many.
Michael Patterson
January 20, 2026 at 14:58Look, I’m all for innovation, but let’s be real: 15-20% VUS? That’s a nightmare. You give someone a report with ‘unknown mutation’ and they Google it and think they’re dying. And then the doctor says ‘we don’t know’ and you’re stuck in limbo for months. This isn’t progress-it’s emotional chaos with a price tag. And don’t even get me started on how many docs don’t even know how to read these reports. We’re putting the cart before the horse.
Madhav Malhotra
January 22, 2026 at 08:47As someone from India, I’m amazed at how fast this is moving. In my village, people still think cancer is a curse. But if this becomes cheap and simple, we can teach communities: ‘It’s not magic, it’s science.’ One blood test to know, to act, to survive. That’s real change.