Anticholinergic Burden Calculator
Medication Risk Assessment Tool
This tool calculates your cumulative anticholinergic burden score based on medications you take. High scores indicate increased risk of cognitive decline. Note: This is for informational purposes only and should not replace professional medical advice.
Your Medications
Anticholinergic Burden Assessment
Many older adults reach for diphenhydramine - the active ingredient in Benadryl - to help them sleep or ease allergy symptoms. It’s cheap, easy to find, and seems harmless. But what if using it every night for years could be quietly affecting your brain? The connection between long-term antihistamine use and dementia isn’t simple, but the warning signs are growing louder.
Not All Antihistamines Are the Same
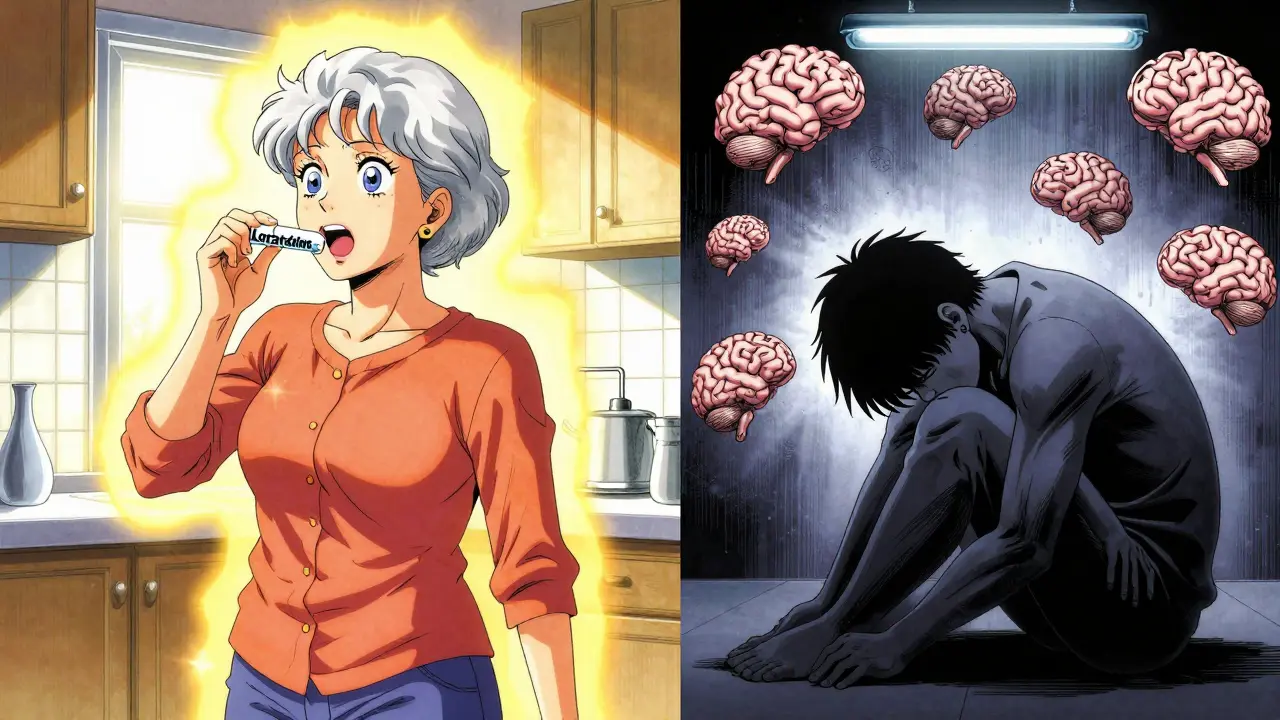
There are two main types of antihistamines: first-generation and second-generation. The difference isn’t just about brand names - it’s about what happens inside your brain.First-generation antihistamines like diphenhydramine, doxylamine, and chlorpheniramine cross the blood-brain barrier. Once there, they block acetylcholine, a key chemical your brain uses for memory, focus, and learning. This is called anticholinergic activity. These drugs were designed to make you drowsy - that’s why they’re in sleep aids. But that same effect can wear down cognitive function over time.
Second-generation antihistamines - like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) - were made to avoid this. They’re engineered to stay out of the brain. They work just as well for allergies without the brain fog. If you’re taking an antihistamine regularly, check the label. If it says "drowsiness may occur," you’re likely on a first-generation drug.
What the Research Really Shows
A 2015 study in JAMA Internal Medicine that tracked over 3,400 older adults for a decade made headlines: people who took strong anticholinergic drugs had a higher chance of developing dementia. At the time, many assumed antihistamines were part of the problem.But follow-up studies painted a more complex picture. A 2019 analysis found that while antidepressants and bladder medications showed clear links to dementia risk, antihistamines did not. The hazard ratio? Exactly 1.00 - meaning no increased risk. Another 2022 study of nearly 9,000 seniors found dementia rates were slightly higher among those taking diphenhydramine, but the difference wasn’t statistically significant.
So why the confusion? Because earlier studies grouped all anticholinergic drugs together. When you separate them, the risk isn’t the same. Antihistamines don’t appear to carry the same danger as drugs like oxybutynin (for overactive bladder) or amitriptyline (for depression). But that doesn’t mean they’re safe.
The Real Problem: Cumulative Exposure
Even if a single dose of diphenhydramine doesn’t hurt, taking it every night for five, ten, or twenty years adds up. Think of it like a slow leak in a boat - you don’t notice it until the water’s up to your knees.The American Geriatrics Society’s 2023 Beers Criteria says it plainly: avoid first-generation antihistamines in adults 65 and older. They’re rated as "Avoid" with the highest level of evidence. Why? Because the brain’s ability to compensate for reduced acetylcholine declines with age. What’s tolerable at 55 might be damaging at 75.
And it’s not just about dementia. Long-term anticholinergic use is linked to confusion, poor balance, urinary retention, and constipation - all of which increase fall risk and hospitalizations in older adults. One 2022 survey found that 42% of adults over 65 regularly used OTC antihistamines for sleep. And 78% had no idea they were taking something with anticholinergic effects.
Why Do People Keep Using Them?
The answer is simple: they work. Diphenhydramine helps people fall asleep fast. It’s easier than waiting weeks for a therapist, cheaper than a sleep study, and doesn’t require a prescription. But it’s a band-aid on a broken bone.On Reddit, a geriatric care manager with 2,400 karma wrote: "83% of my clients over 70 are taking diphenhydramine nightly. They think it’s harmless because it’s over-the-counter." That’s the myth we need to break.
Many doctors didn’t get updated training on anticholinergic risks. Patients aren’t warned. Labels still say "may cause drowsiness," not "may increase dementia risk over time." The FDA hasn’t required stronger warnings on OTC products, even though they added dementia warnings to prescription anticholinergics in 2021.
What Should You Do Instead?
If you’re taking diphenhydramine for sleep or allergies, here’s what to consider:- Switch to second-generation antihistamines. Loratadine, cetirizine, and fexofenadine work just as well for allergies and don’t cross into the brain.
- For insomnia, try CBT-I. Cognitive Behavioral Therapy for Insomnia has a 70-80% success rate in older adults. It’s not a pill - it’s a set of habits that retrain your brain to sleep naturally. The problem? Wait times for therapists are long, and Medicare only covers about $85-$120 per session.
- Ask about low-dose doxepin. This prescription sleep aid (brand name Silenor) has minimal anticholinergic effects and is approved for long-term use in older adults. It’s not cheap, but it’s safer than Benadryl.
- Review all your meds every six months. The American Academy of Neurology recommends this. Many older adults take 5-10 medications. Add up their anticholinergic burden using the ACB scale - diphenhydramine scores a 3 (highest), while second-gen antihistamines score 0.

What’s Changing Now?
The tide is turning. Global sales of first-generation antihistamines dropped 24% between 2015 and 2022. Second-gen sales grew by 18%. More people are asking questions. Pharmacies are starting to flag high-risk combinations.Big studies are underway. The ABCO study, launched in 2023 with $4.2 million in NIH funding, is tracking 5,000 people over ten years with detailed medication logs and annual brain scans. Early results from the UK Biobank suggest that when you control for underlying sleep disorders, antihistamine use doesn’t increase dementia risk. That’s important - it means the problem might not be the drug itself, but the condition it’s treating.
The FDA is reviewing all anticholinergic medications. The American Geriatrics Society’s 2024 Beers Criteria update, due in June, will likely add even more specific warnings. Meanwhile, the European Medicines Agency already requires patient leaflets to mention "potential long-term cognitive effects."
The Bottom Line
You don’t need to panic if you’ve taken Benadryl for years. But you do need to act now. If you’re still using first-generation antihistamines regularly - especially for sleep - talk to your doctor. Ask: "Is this the safest option?" and "Are there alternatives that won’t affect my brain?"There’s no magic pill for better sleep or allergy relief that’s both safe and effective. But there are better choices. Second-gen antihistamines. Behavioral therapy. Prescription alternatives with lower risk. The goal isn’t to eliminate all medications - it’s to stop using the ones that silently wear down your mind.
Don’t wait for a diagnosis to change your habits. Your brain doesn’t give you warning signs until it’s too late. Start today. Check your medicine cabinet. Read the labels. Ask questions. You’re not just protecting your memory - you’re protecting your future self.




Alvin Bregman
January 15, 2026 at 03:01ive been taking zyrtec for years and never had a problem my grandpa took benadryl every night for 20 years and hes 89 and still remembers my birthday so dont scare people with stats that dont add up
Sarah -Jane Vincent
January 15, 2026 at 23:07oh here we go again the big pharma shills are out in full force. you think they really care about your brain? theyre just trying to sell you expensive second-gen drugs so they can keep raking in billions. diphenhydramine has been around since 1946 and if it was that dangerous do you think the fda wouldve let it stay on shelves for 80 years? theyre just pushing this narrative because they want you to pay for a prescription sleep aid instead of a dollar store solution. wake up people.
Henry Sy
January 17, 2026 at 09:41man i used to chow down on benadryl like candy back in college just to crash hard. now im 62 and i swear i feel like my brain is made of wet cardboard some days. i switched to claritin last year and holy hell the fog lifted. i forgot how good it felt to read a book without needing a nap halfway through. dont get me wrong i still dont trust the medical establishment but this one? this one actually checked out.
Anna Hunger
January 19, 2026 at 03:51It is imperative to emphasize that the American Geriatrics Society’s Beers Criteria explicitly categorizes first-generation antihistamines as potentially inappropriate medications for individuals aged 65 and older. The evidence base supporting this recommendation is robust and grounded in longitudinal clinical data. Dismissing these findings as pharmaceutical propaganda undermines evidence-based geriatric care and endangers vulnerable populations.
says haze
January 20, 2026 at 08:33the real tragedy here is not the antihistamines-it’s the societal collapse that has rendered sleep and allergy management into pharmaceutical band-aids. we’ve outsourced our biology to convenience. we’ve turned our bodies into machines that need firmware updates. diphenhydramine is not the villain-it’s the symptom. the real disease is a culture that values speed over sustainability, pills over presence, and silence over understanding.
Jason Yan
January 21, 2026 at 01:02look i get why people use benadryl. i used to too. i was exhausted from working two jobs and raising a kid alone. sleep wasnt a luxury it was a survival tactic. but after my mom had a fall because she was dizzy from her nightly dose i started digging. turns out she was on three other meds with anticholinergic effects too. we switched her to cetirizine and started cbt-i and now shes sleeping better than shes slept in 15 years. its not about fear its about awareness. you dont have to be perfect just curious.
shiv singh
January 21, 2026 at 11:53you americans are so weak. in india we take antihistamines every day and no one gets dementia. you people are so obsessed with your brains you forget how to live. my uncle took diphenhydramine for 30 years and he still runs his own shop and argues with everyone on whatsapp. stop being so scared of everything. your fear is making you sick not the medicine.
Robert Way
January 21, 2026 at 13:12wait so if i take claritin its safe but if i take benadryl im gonna get dementia? but what if i take both? does that cancel out? or make it worse? i just need to sleep and i dont have time to read all this
Sarah Triphahn
January 22, 2026 at 17:02you people are pathetic. you take drugs because youre too lazy to fix your sleep schedule. you dont want to wake up at 5am to get sunlight. you dont want to stop scrolling at 10pm. you just want a chemical crutch. diphenhydramine isnt the problem. you are. stop blaming medicine for your poor choices.
Vicky Zhang
January 24, 2026 at 13:45i just want to say thank you for writing this. my mom was on benadryl for sleep for 12 years and we never knew. when we switched her to zyrtec and started a bedtime routine she started remembering our names again. she laughed the other day and said she felt like herself for the first time in a decade. this post saved her. please keep sharing this info. so many people are just waiting for someone to tell them its okay to ask for help.
Allison Deming
January 26, 2026 at 12:10While it is tempting to reduce complex neurocognitive outcomes to single-agent causality, the epidemiological data remains inconclusive. The absence of statistical significance in several cohort studies does not equate to biological safety. The precautionary principle must govern clinical decision-making, particularly in populations with diminished neuroplasticity. Furthermore, the normalization of OTC anticholinergic use reflects a broader public health failure in medication literacy.
Susie Deer
January 28, 2026 at 10:26usa is weak. other countries dont care about this stuff. we got real problems like crime and borders. this is just another woke medical scare. benadryl is fine. stop making everything a crisis
TooAfraid ToSay
January 30, 2026 at 01:55you know what they dont tell you? the real reason they want you off benadryl? because it’s cheap. they want you on their fancy $200/month sleep meds. they’re scared of a $5 bottle that works better than their patents. this is capitalism not medicine. they dont care if you sleep better they care if you spend more
Dylan Livingston
January 30, 2026 at 18:35how ironic that the same people who scream about corporate greed are now begging pharmaceutical companies to tell them what to take. you want autonomy? then stop outsourcing your health decisions to a reddit post. go to a doctor. read the actual studies. stop letting influencers tell you your brain is dying because you took a pill once. you’re not a victim. you’re a consumer. and you’re being manipulated by both sides.