High cholesterol isn’t something you feel. No pain. No warning signs. Just a quiet, slow buildup in your blood that can lead to a heart attack or stroke without warning. That’s why it’s called a silent killer. By the time symptoms show up-chest pain, shortness of breath, numbness in limbs-the damage is often already done. In 2023, nearly 94 million American adults had total cholesterol levels above 200 mg/dL. In Australia, the picture isn’t much different. One in three adults over 45 has high cholesterol, and many don’t even know it.
What Exactly Is Hypercholesterolemia?
Hypercholesterolemia is the medical term for high cholesterol in your blood. Cholesterol isn’t bad by itself. Your body needs it to build cells, make hormones, and digest food. The problem comes when there’s too much of the wrong kind-low-density lipoprotein, or LDL. That’s the "bad" cholesterol. When LDL levels rise, it sticks to the walls of your arteries, forming plaque. Over time, this narrows your blood vessels, restricts blood flow, and increases your risk of heart disease, heart attack, and stroke.
The American Heart Association defines normal total cholesterol as under 200 mg/dL. Borderline high is 200-239 mg/dL. Anything above 240 mg/dL is considered high. But the real red flag is LDL. Levels above 190 mg/dL are classified as severe hypercholesterolemia. At this point, your risk of heart disease skyrockets-even if you’re young and active.
Familial Hypercholesterolemia: It’s Not Just About Diet
Not everyone with high cholesterol eats too much butter or fries. About 1 in 250 people worldwide have a genetic condition called familial hypercholesterolemia (FH). This isn’t a lifestyle issue-it’s inherited. If one parent has it, you have a 50% chance of getting it too.
People with heterozygous FH (one faulty gene) often have LDL levels between 190 and 400 mg/dL from birth. Homozygous FH (two faulty genes) is rarer but far more dangerous. These individuals can have LDL levels over 450 mg/dL. Without treatment, they often suffer heart attacks before age 20.
Physical signs can give it away. Yellowish fatty deposits around the eyelids (xanthelasmas) or thickened tendons in the heels or knuckles (tendon xanthomas) are telltale signs. If you or a family member has these, get tested. FH is underdiagnosed-only about 10% of people with it know they have it.
What Causes High Cholesterol Besides Genetics?
If you don’t have FH, your high cholesterol likely comes from lifestyle or other health conditions. The most common culprits:
- Unhealthy diet: Saturated fats (red meat, full-fat dairy, fried foods) and trans fats (processed snacks, baked goods) raise LDL. Even though dietary cholesterol (like eggs) has less impact than once thought, the overall pattern matters.
- Lack of movement: Physical inactivity lowers HDL (the "good" cholesterol) and increases LDL.
- Obesity: Excess weight, especially around the waist, changes how your body handles fat and cholesterol.
- Diabetes: About 68% of people with type 2 diabetes have abnormal cholesterol levels. High blood sugar damages blood vessels and makes LDL more likely to stick.
- Thyroid problems: An underactive thyroid (hypothyroidism) slows metabolism and can raise cholesterol by 15-20%.
- Medications: Some diuretics, beta-blockers, and steroids can increase LDL levels.
It’s not just one thing. Most people have a mix-poor diet, low activity, and a hidden health condition working together.
How Is It Diagnosed?
You can’t feel high cholesterol. You can only know it through a simple blood test-a lipid panel. This checks total cholesterol, LDL, HDL, and triglycerides.
Here’s what the numbers mean:
| Level Type | Desirable | Borderline High | High |
|---|---|---|---|
| Total Cholesterol | Under 200 mg/dL | 200-239 mg/dL | 240 mg/dL and above |
| LDL (Bad) | Under 100 mg/dL | 100-129 mg/dL | 130 mg/dL and above |
| HDL (Good) | 60 mg/dL and above | 40-59 mg/dL | Below 40 mg/dL |
| Triglycerides | Under 150 mg/dL | 150-199 mg/dL | 200 mg/dL and above |
The good news? You don’t need to fast anymore for a standard lipid panel. Just show up. Your doctor can order it during a routine check-up. The U.S. Preventive Services Task Force recommends testing for all adults between 40 and 75. But if you have a family history of early heart disease or FH, get tested earlier-even in your 20s.
Treatment: It’s Not Just About Statins
Once diagnosed, treatment depends on your risk level. For most people, it starts with lifestyle changes. But for those with FH or existing heart disease, medication is non-negotiable.
Statins are the first-line treatment. Drugs like atorvastatin and rosuvastatin can cut LDL by 50% or more. They’re safe, affordable, and proven to prevent heart attacks. But about 1 in 5 people can’t tolerate them due to muscle pain or other side effects.
If statins don’t work or aren’t an option, there are alternatives:
- Ezetimibe: Blocks cholesterol absorption in the gut. Lowers LDL by about 18%.
- PCSK9 inhibitors: Injectable drugs like alirocumab and evolocumab. These can slash LDL by another 50-60% on top of statins. Used for FH or very high-risk patients.
- Inclisiran (Leqvio): A newer shot given just twice a year. It works at the genetic level to reduce LDL production. Approved in 2021, it’s a game-changer for adherence.
People with FH often need a triple combo: high-dose statin + ezetimibe + PCSK9 inhibitor. It sounds intense, but for them, it’s life-saving. Studies show that lowering LDL below 70 mg/dL can stop plaque growth-and even reverse it over time.
Lifestyle Changes That Actually Work
Medication helps, but it doesn’t replace healthy habits. The best outcomes come when drugs and lifestyle work together.
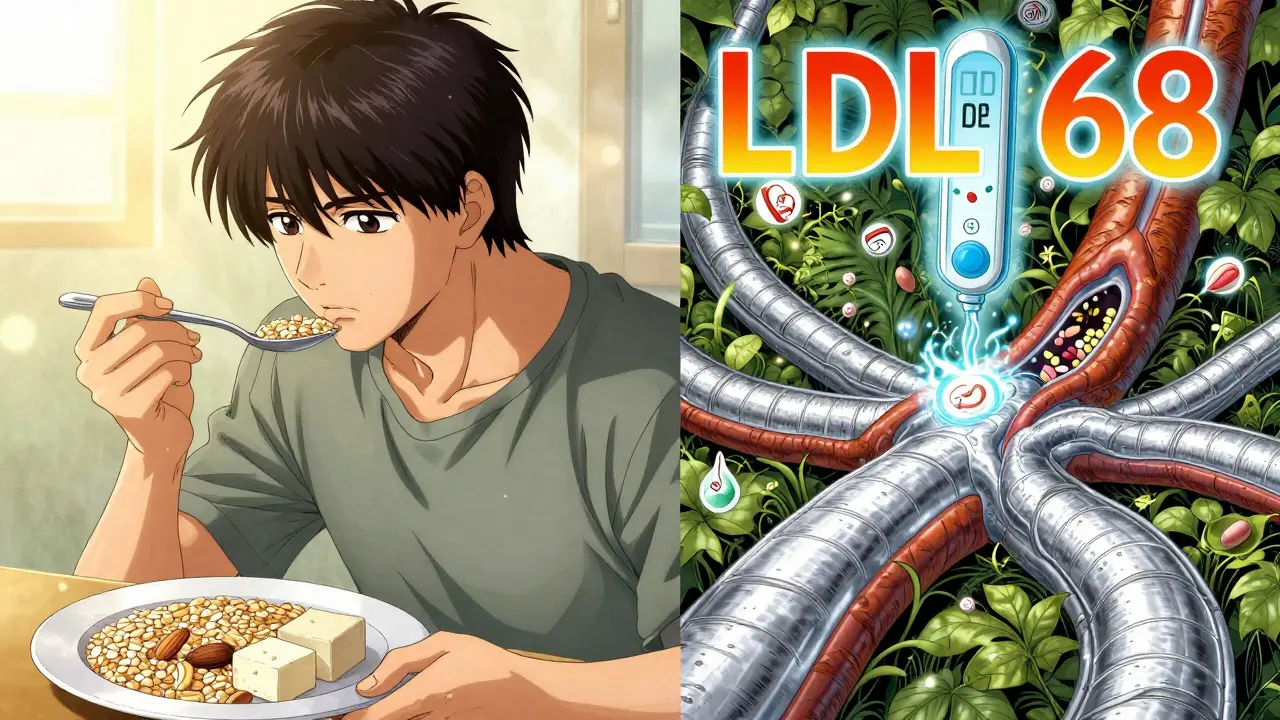
The Portfolio Diet is one of the most effective approaches. It’s not a fad-it’s science-backed. It combines four key foods:
- Plant sterols: Found in fortified margarines and supplements. Block cholesterol absorption.
- Soluble fiber: Oats, beans, lentils, apples, psyllium. Binds cholesterol in the gut.
- Nuts: Almonds, walnuts, peanuts. About a handful a day lowers LDL.
- Soy protein: Tofu, edamame, soy milk. Replaces animal protein.
Studies show this diet can reduce LDL by 20-30%-similar to low-dose statins. And it works even better when you cut out ultra-processed foods and added sugars.
Exercise matters too. Just 30 minutes of brisk walking five days a week can raise HDL and lower triglycerides. You don’t need to run a marathon. Consistency beats intensity.

Why So Many People Don’t Get Treated
Here’s the frustrating part: even when people are diagnosed, many don’t stick with treatment. Only about half of people on statins are still taking them after a year. Why?
- Side effects: Muscle aches are common, but often exaggerated. Many people stop thinking it’s the drug, when it’s not.
- Feeling fine: If you don’t feel sick, you don’t think you need the pill.
- Cost and access: PCSK9 inhibitors can cost over $10,000 a year. Even with insurance, co-pays are high.
- Gender and racial gaps: Women and Black adults are less likely to be prescribed statins-even when they meet the criteria.
In Australia, similar gaps exist. Many people rely on natural remedies or ignore the problem until it’s too late. But high cholesterol doesn’t wait. Every year you delay treatment, your risk grows.
The Future of Cholesterol Management
The field is changing fast. Genetic testing is becoming more common. Polygenic risk scores-based on hundreds of small genetic variations-can now identify people at risk even if they don’t have FH. This means we can start prevention earlier, sometimes in childhood.
Doctors are also moving away from one-size-fits-all targets. Instead of just aiming for "under 100," they’re looking at your overall risk: age, blood pressure, smoking, diabetes, family history. Your LDL goal is personalized.
And policy is catching up. Australia’s National Heart Foundation now recommends statins for people with a 10-year risk of heart disease over 10%. That’s lower than in many other countries. It’s about preventing disease before it starts.
What You Should Do Right Now
If you’re over 40, get your cholesterol checked. If you’re younger but have a family history of early heart disease, get tested anyway. Don’t wait for symptoms. Don’t assume you’re fine because you’re active or eat "healthy."
- Ask your doctor for a lipid panel.
- If your LDL is above 130, talk about whether you need medication.
- If you have tendon xanthomas or xanthelasmas, insist on genetic testing for FH.
- Start eating more oats, beans, nuts, and plant sterols. Cut back on fried foods and processed snacks.
- Move every day-even a 20-minute walk counts.
High cholesterol is preventable. It’s treatable. But it won’t fix itself. The longer you wait, the harder it gets. And the cost-both in health and money-is far higher than most people realize.
Don’t let silence be your only symptom. Get tested. Take action. Your future heart will thank you.
Can you have high cholesterol and still be thin?
Yes. Cholesterol levels are influenced more by genetics and diet than body weight. Many thin people have high LDL due to familial hypercholesterolemia or a diet high in saturated fats. You can’t judge cholesterol by appearance.
Do eggs raise cholesterol?
For most people, eating one egg a day doesn’t significantly raise blood cholesterol. The bigger issue is what you eat with it-like bacon, buttered toast, or fried sides. The overall diet pattern matters more than single foods.
Can you reverse plaque buildup from high cholesterol?
Yes, with aggressive treatment. Studies show that lowering LDL below 70 mg/dL with statins and PCSK9 inhibitors can shrink plaque over time. The key is early, sustained intervention-not waiting until after a heart attack.
How often should you check your cholesterol?
If your levels are normal and you have no risk factors, check every 4-6 years after age 20. If you’re over 40, have high cholesterol, or have diabetes or high blood pressure, get tested annually or as your doctor recommends.
Are natural supplements like red yeast rice safe?
Red yeast rice contains a compound similar to statins and can lower LDL. But it’s not regulated like prescription drugs. Doses vary, and it can cause the same side effects as statins-muscle damage, liver stress. Talk to your doctor before using it.
Is high cholesterol hereditary?
Yes, in about 1 in 250 people, it’s caused by familial hypercholesterolemia-an inherited condition. If a parent or sibling had early heart disease (before age 55 for men, 65 for women), you should be tested.
High cholesterol doesn’t care if you’re busy, stressed, or think you’re too young to worry. It’s a slow, silent threat-but one you can control. The tools are here. The science is clear. What’s left is action.





Kevin Motta Top
December 18, 2025 at 23:48Just got my lipid panel back-LDL at 142. Doctor said "mildly elevated." I said "so I’m not dead yet?" He laughed. Point is, you don’t need to panic. Just move more, eat less junk, and get checked again in six months. No statins needed. Yet.
Henry Marcus
December 19, 2025 at 16:58THEY DON’T WANT YOU TO KNOW THIS-cholesterol is a LIE! The pharmaceutical industry invented LDL to sell statins! Your body makes cholesterol because it’s ESSENTIAL! They’re poisoning your liver to keep you dependent! Look up the 1977 McGovern hearings-THEY ADJUSTED THE NUMBERS TO CREATE A PANIC! You think your doctor cares? They get kickbacks from Big Pharma! Wake up!!
Carolyn Benson
December 19, 2025 at 18:10It’s not about cholesterol. It’s about control. The medical-industrial complex needs you afraid. Fear sells pills. Fear sells tests. Fear sells diets. You think your body is broken? Or do you think you’ve been taught to distrust your own biology? We’ve been conditioned to outsource health to strangers in white coats who’ve never fasted, never walked barefoot, never listened to their own pulse. Cholesterol is just the latest scapegoat for a society that’s lost its way.
Maybe the real problem isn’t your LDL-it’s that you’ve forgotten how to live.
Chris porto
December 19, 2025 at 18:22I used to think high cholesterol was just about eating too much bacon. Then my dad had a heart attack at 52-no weight issues, no smoking, just genetics. We got tested. Turns out, I’ve got the same gene. I didn’t want to believe it. But now I take a low-dose statin and eat oats every morning. It’s not glamorous. But it’s working. You don’t have to be perfect. Just consistent.
Aadil Munshi
December 20, 2025 at 12:34Oh wow, another article that treats cholesterol like it’s a villain. Let me guess-you also think sugar isn’t the real culprit? And that exercise alone fixes everything? Lol. The truth is, most people don’t have FH. They just eat processed food like it’s oxygen. And then they blame their genes. Meanwhile, in India, my grandma ate ghee daily, walked 8km a day, and lived to 98. No statins. Just life. Maybe the problem isn’t cholesterol-it’s the modern diet that’s killing us, not the cholesterol itself.
Frank Drewery
December 21, 2025 at 13:15I was diagnosed with high LDL last year. I was terrified. Then I started walking after dinner, swapped my cereal for oats with flaxseed, and cut out the soda. Six months later, my LDL dropped 40 points. I didn’t need a drug. I just needed to make small changes and stick with them. You got this. One step at a time.
Danielle Stewart
December 22, 2025 at 11:12Hey-just wanted to say this article is SO important. So many people think if they’re thin, they’re fine. Nope. I’m 32, size 4, and my LDL was 189. No symptoms. No idea. I cried when I found out. But I’m on it now. Eating more beans. Walking. Talking to my doctor. You’re not alone. And you’re not too late. Start today.
mary lizardo
December 23, 2025 at 11:04It is, regrettably, a matter of public record that the American Heart Association's guidelines have been systematically compromised by pharmaceutical lobbying. The arbitrary thresholds for "high" cholesterol were lowered in 2013 without sufficient peer-reviewed evidence, thereby pathologizing millions of otherwise healthy individuals. Furthermore, the assertion that plaque regression is achievable via LDL reduction below 70 mg/dL is extrapolated from a select cohort of high-risk patients in controlled trials-not representative of the general population. One must question the epistemological validity of such medical pronouncements.
jessica .
December 23, 2025 at 13:46They say cholesterol is bad but they pump chemicals into our food and water and then sell us pills to fix it. It’s a scam. I’m not taking statins. I eat butter. I eat eggs. I drink milk. I’m not some weak American. My grandpa lived to 95 on bacon and lard. They want you scared so you’ll obey. I won’t. I’m American. I choose freedom. Even if it kills me.
Ryan van Leent
December 24, 2025 at 20:28Everyone’s so obsessed with cholesterol but nobody talks about how much stress kills you. I work 80 hours a week, sleep 4 hours, eat takeout every night, and my numbers are fine. Meanwhile, my coworker who eats quinoa and yoga every day has LDL at 190. So what’s the real problem? Maybe it’s not what you eat. Maybe it’s that you’re just tired and broken. Nobody tells you that.
Sajith Shams
December 26, 2025 at 12:18Let me break this down for you. The article mentions FH but doesn’t explain that 90% of cases are missed because doctors don’t screen. In India, we have a saying: "If your father died before 50, you’re already dead." We test our kids at 10. Here? You wait until you’re 50 and have a heart attack. That’s not medicine. That’s negligence. And don’t even get me started on how they ignore triglycerides. You can have perfect LDL and still be a walking time bomb if your triglycerides are through the roof. Nobody talks about that.
Adrienne Dagg
December 26, 2025 at 20:40Just got my results and my LDL is 145 😭 I was so scared but then I started eating more almonds and I’m feeling better already 🙌 I’m not giving up! 💪 #cholesterolwarrior #healthiswealth
Chris Davidson
December 27, 2025 at 18:43Statins work. End of story. If you don’t like it, don’t take them. But don’t pretend the science isn’t there. The data is clear. Lower LDL = fewer heart attacks. You can debate the numbers all you want but people are still dying. And you’re not helping by spreading doubt. Just get tested. Take the pill. Or don’t. But stop pretending you know better than 40 years of clinical trials.
Isabel Rábago
December 28, 2025 at 01:10My mom had FH. She was 28 when she had her first heart attack. She didn’t even smoke. She was thin. She ate salads. But her LDL was 380. They didn’t diagnose her until it was too late. Now I get tested every year. I’m 26. I take ezetimibe. I eat the Portfolio Diet. I don’t care if it’s boring. I’d rather be alive than "natural." This isn’t a trend. It’s survival.
Anna Sedervay
December 29, 2025 at 13:49It’s fascinating how the medical establishment has weaponized cholesterol to pathologize normal human physiology. The notion that a lipid molecule can be inherently "bad" is a reductive anthropocentric fallacy. Evolution did not design the human body to be free of cholesterol-it designed it to survive famine, not the modern supermarket. The real tragedy is not hypercholesterolemia-it’s the abandonment of ancestral metabolic wisdom in favor of pharmacological band-aids. I, for one, have returned to ancestral fats, intermittent fasting, and cold exposure. My LDL? 112. My peace of mind? Priceless.
Chris porto
December 31, 2025 at 11:43Chris Davidson’s comment hit hard. I used to be the guy who thought "I’m fine" until my dad dropped. Now I take my statin every morning like brushing my teeth. No drama. No guilt. Just a habit. If you’re on the fence, just try it for three months. If your muscles hurt, talk to your doctor about switching. But don’t quit because you’re scared. Your future self will thank you.