Managing diabetes isn’t just about pills or insulin-it’s about movement. If you have type 1 or type 2 diabetes, regular physical activity is one of the most powerful tools you have to bring your blood sugar down, improve insulin sensitivity, and reduce your risk of heart disease. And it’s not about running marathons. It’s about consistent, smart movement that fits your life.
Why Exercise Lowers Blood Sugar
When you move, your muscles use glucose for energy. That’s it. No insulin needed. This is especially helpful for people with type 2 diabetes, whose bodies don’t use insulin well. Exercise makes your muscles more sensitive to insulin, so your body can do more with less. Even a 20-minute walk after dinner can slash your post-meal blood sugar spike by up to 30%.Studies show that people who stick with regular exercise lower their HbA1c-a key measure of long-term blood sugar control-by 0.5% to 0.7%. That’s similar to the effect of some diabetes medications. And the benefits don’t stop there. Regular activity cuts heart disease risk by 31%, reduces belly fat, and helps you sleep better.
The Science-Backed Exercise Plan for Diabetes
The American Diabetes Association, the American College of Sports Medicine, and other leading groups agree on one thing: a mix of aerobic and strength training works best. Here’s what the evidence says you should do.- Aerobic exercise: Aim for 150 minutes per week of moderate activity-like brisk walking, cycling, or swimming. That’s 30 minutes, five days a week. If you’re short on time, 75 minutes of vigorous activity (like jogging or fast cycling) works too. The key? Don’t skip more than two days in a row. The insulin-sensitizing effect fades after 48 hours.
- Resistance training: Do strength exercises two to three times a week. Focus on all major muscle groups: legs, back, chest, arms, and core. Use weights or resistance bands. Do 2-4 sets of 8-15 reps at a weight that feels challenging by the last rep. This builds muscle, which burns more glucose-even when you’re resting.
- Break up sitting: If you sit for long hours, get up every 30 minutes. Walk for 3 minutes. Do bodyweight squats or heel raises. This simple habit cuts post-meal glucose by 24% and insulin by 20% compared to staying seated all day.
Combined training-mixing cardio and strength-is the gold standard. One study found it lowers HbA1c 0.56% more than cardio alone and 0.47% more than strength alone. If you only have time for one, do both over the week. Don’t pick one and ignore the other.
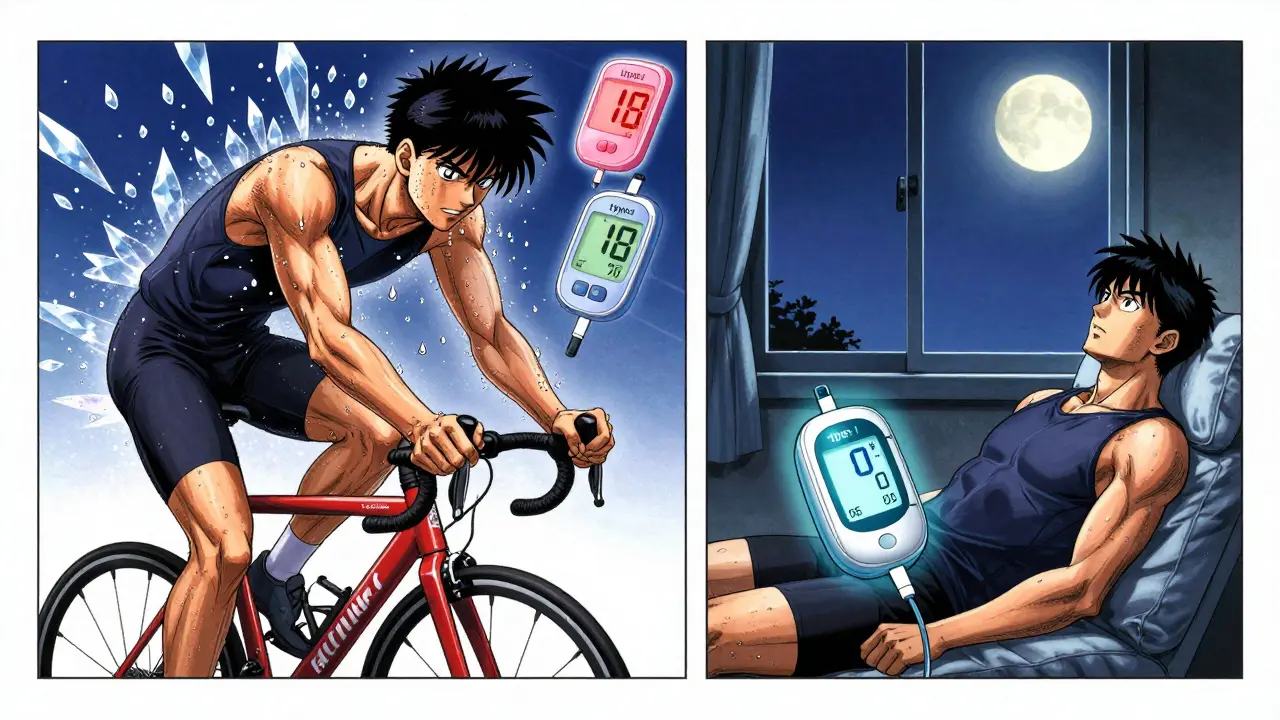
High-Intensity Interval Training (HIIT): Faster Results, But Watch Out
HIIT-short bursts of hard effort followed by rest-is gaining attention. A 20-minute session of cycling hard for 1 minute, then pedaling easy for 1 minute, repeated 10 times, can give you the same blood sugar benefits as 40 minutes of steady walking. It saves time. It burns fat fast. And it improves insulin sensitivity more per minute than moderate exercise.But it’s not for everyone. HIIT can cause a temporary spike in blood sugar after exercise, especially in type 1 diabetes. About 35% of people with type 1 see their glucose rise after intense workouts. It can also be risky if you have nerve damage, eye problems from diabetes, or heart issues. If you’re new to exercise or over 60, start with moderate walking or cycling first. Save HIIT for later, after you’ve built a base.
How to Check Your Blood Sugar Before, During, and After Exercise
Exercise affects blood sugar differently for everyone. You need to know your numbers.- Before exercise: Test your blood sugar 15-30 minutes before you start. If it’s below 100 mg/dL, eat 15-30 grams of fast-acting carbs-like a banana, 4 glucose tablets, or half a cup of juice. If it’s above 250 mg/dL and you have ketones (test with urine strips), don’t exercise. You risk ketoacidosis.
- During exercise: If you’re doing more than an hour of activity, check every 30 minutes. Carry fast-acting carbs with you. Eat 15 grams every 30 minutes if you’re active for a long time.
- After exercise: Blood sugar can drop for up to 24 hours. Keep checking. Have a small snack with protein and carbs after your workout, especially if you took insulin. Nighttime lows are common-set an alarm if you’re at risk.
People using insulin pumps should lower their basal rate by 50% one hour before exercise and keep it low during activity. Those on insulin injections may need to reduce their mealtime dose by 20-40% for moderate activity. Always talk to your doctor before changing doses.
What to Do If Your Blood Sugar Drops During Exercise
Hypoglycemia during exercise is real. About 25% of people with type 1 diabetes experience it. Symptoms include shakiness, sweating, dizziness, confusion, or sudden fatigue.Here’s what to do:
- Stop exercising immediately.
- Test your blood sugar.
- If it’s below 70 mg/dL, consume 15 grams of fast-acting carbs.
- Wait 15 minutes. Test again.
- If still low, repeat. Don’t resume exercise until your sugar is above 100 mg/dL.
Keep glucose tabs, juice boxes, or hard candies in your gym bag, car, and desk drawer. Don’t wait until you feel bad to have them handy.
Exercise Tips for Different Types of Diabetes
Type 1 Diabetes
Your body doesn’t make insulin. So exercise can cause wild swings. You need to be extra careful with timing and dosing. Use a continuous glucose monitor (CGM) if you can. It shows trends, not just numbers. Many people find their blood sugar drops during cardio but rises after weightlifting. Adjust your insulin and snacks accordingly. Talk to your endocrinologist about setting up a personalized plan.
Type 2 Diabetes
You’re likely insulin resistant. Exercise is your best medicine. Start slow. Walking 3 miles a day (about 18.2 km/week) can improve your body’s response to insulin-even without losing weight. You don’t need to run. Just move more. Strength training is especially powerful here. It builds muscle, which soaks up glucose like a sponge.
Gestational Diabetes
If you’re pregnant, avoid high-impact activities like jumping or heavy lifting. Stick to walking, swimming, or prenatal yoga. Keep your heart rate under 140 bpm. Stay hydrated. Check your blood sugar before and after each session. Many women find that 30 minutes of walking after meals keeps their numbers steady.

Why Most People Quit-And How to Stick With It
The hard truth? Two out of three people with diabetes drop out of exercise programs within six months. Why? Time, lack of support, and feeling overwhelmed.Here’s how to beat the odds:
- Find a buddy. Walk with a friend or join a local diabetes fitness group.
- Make it part of your routine. Schedule workouts like appointments.
- Start small. Five minutes a day is better than nothing. Build up slowly.
- Track progress. Use a journal or app. Note how you feel, not just your numbers.
- Celebrate non-scale wins: better sleep, more energy, clothes fitting better.
Medicare and many insurance plans now cover diabetes prevention programs that include exercise coaching. Ask your doctor if you qualify. These programs have been shown to cut diabetes risk by 14% and help people lose over 5% of their body weight.
What’s Next? Technology and Personalization
The future of diabetes and exercise is personal. Researchers are testing AI apps that give real-time advice based on your glucose trends, workout type, and insulin levels. Early results show these tools can reduce exercise-related highs and lows by 40%.Genetic testing is also being studied to predict who responds best to HIIT vs. walking. In five years, your phone might tell you: "Your glucose is dropping fast-take 10g carbs now and lower your basal by 20% for the next hour."
For now, the best tool you have is consistency. Move daily. Monitor your numbers. Adjust as needed. And don’t wait for perfection. A walk after dinner, a few squats while brushing your teeth, taking the stairs-these all add up.
Can I exercise if my blood sugar is high?
If your blood sugar is above 250 mg/dL and you have ketones in your urine, don’t exercise. You risk diabetic ketoacidosis. If your sugar is high but you have no ketones, light activity like walking may help bring it down. Test again after 30 minutes. If it’s still rising, wait and consult your doctor.
Is walking enough for type 2 diabetes?
Yes, walking is one of the most effective exercises for type 2 diabetes. Studies show that walking 3 miles a day (about 18.2 km per week) improves insulin sensitivity and lowers HbA1c-even without weight loss. Combine it with strength training twice a week for even better results.
Should I take my insulin before exercising?
It depends. If you’re on insulin, you may need to reduce your dose before exercise to avoid low blood sugar. For moderate activity, reduce your mealtime insulin by 20-40%. For high-intensity workouts, reduce by 30-60%. People using insulin pumps should lower their basal rate by 50% one hour before and during exercise. Always talk to your healthcare provider before making changes.
What’s the best time of day to exercise with diabetes?
There’s no single best time. Many people find morning exercise helps control blood sugar all day. Others prefer post-meal walks to prevent spikes. The key is consistency. Choose a time you can stick with. If you’re on insulin, avoid exercising during peak insulin action unless you’ve adjusted your dose.
Can exercise reverse type 2 diabetes?
Exercise alone won’t cure type 2 diabetes, but when combined with weight loss and healthy eating, it can lead to remission. Studies show that losing 5-10% of body weight and exercising 150 minutes per week can put type 2 diabetes into remission for many people-meaning blood sugar returns to normal without medication.
Final Thoughts: Move More, Live Better
You don’t need a gym membership or fancy gear. You need to move. Every day. Even a little. Your body responds to movement-not perfection. Start where you are. Walk around the block. Do chair squats while watching TV. Take the stairs. Over time, these small actions add up to better blood sugar control, more energy, and fewer complications.Diabetes doesn’t have to slow you down. With the right plan, exercise can be your strongest ally.



Andrea Di Candia
December 23, 2025 at 06:12Just wanted to say this post hit different. I’ve been living with type 2 for 8 years, and the moment I started doing 15 minutes of bodyweight squats after dinner, my fasting numbers dropped like a rock. No magic pills, no supplements-just movement. It’s not about being perfect. It’s about showing up, even when you’re tired. I used to think exercise was for athletes. Turns out, it’s for people who want to live.
Still fighting the urge to skip it some days. But now I remind myself: my future self is begging me to move.
Thank you for writing this. It felt like someone finally spoke my language.
Dan Gaytan
December 24, 2025 at 07:03THIS. I’ve been doing the 30-min walk after dinner for 6 months now. My A1c dropped from 7.8 to 6.1. I didn’t even lose weight, but my energy? Night and day. 🙌
Also, the part about breaking up sitting? Game changer. I set a timer on my phone to stand up every 30 mins. Now I do calf raises while brushing my teeth. Weird? Maybe. Effective? Absolutely.
Keep sharing this stuff. People need to hear it from real life, not just doctors.
Usha Sundar
December 24, 2025 at 15:34I tried walking after dinner. My glucose went up. So I stopped. Guess I’m just broken.
Jeffrey Frye
December 25, 2025 at 11:02Let’s be real-this post is full of ‘science-backed’ fluff. The 0.5% HbA1c drop? That’s statistically insignificant for most people. And HIIT being ‘risky’? That’s just fearmongering. You’re telling people to avoid intensity because they might spike? What about the 65% who don’t? Why not mention that exercise-induced hyperglycemia is often temporary and adaptive?
Also, the insulin adjustment advice is dangerously oversimplified. No one should be tweaking basal rates without a CDE. This reads like a wellness blog dressed as medical advice.
Diana Alime
December 25, 2025 at 20:49Okay but why is everyone acting like exercise is the holy grail? I’ve been walking 5k every day for 2 years. My sugar is still all over the place. Meanwhile my cousin who takes metformin and eats keto? Her numbers are perfect. Maybe the real fix is just… not eating carbs?
Also, I tried HIIT once. My heart felt like it was gonna explode. I’m 54. I don’t need to be a warrior. I need to not pass out on the treadmill.
Also also-why does everyone assume we’re all fit enough to do squats? Some of us have bad knees. Just sayin’.
Bhargav Patel
December 27, 2025 at 00:02The notion that physical activity is a panacea for metabolic dysfunction betrays a fundamental misunderstanding of physiological complexity. While it is empirically evident that muscular contraction facilitates glucose uptake independent of insulin, to ascribe therapeutic primacy to movement alone is to reduce a multifactorial pathology to a mechanistic binary.
The body is not a circuit board; it is a dynamic, adaptive system wherein hormonal feedback loops, circadian rhythms, and genetic predispositions interact in non-linear fashion. To prescribe a rigid regimen of 150 minutes weekly-however well-intentioned-is to impose a colonial model of health onto a deeply individualized condition.
One must ask: Is the goal compliance, or is it resilience? The former is quantifiable; the latter, sacred. Perhaps the truest exercise is not the stride, but the sustained, compassionate attention one pays to one’s own bodily signals-regardless of the glucometer’s verdict.
Let us not mistake movement for meaning. The body remembers what the data cannot capture.
Joe Jeter
December 27, 2025 at 09:45Oh great. Another ‘exercise fixes everything’ cultist. You know what else lowers blood sugar? Fasting. Ketosis. Intermittent fasting. Not walking. Not squats. Not ‘moving more.’
And why does no one ever talk about the fact that insulin resistance is caused by excess insulin? You’re telling people to move more to use up glucose… but you’re not telling them to stop flooding their system with carbs and insulin.
Also, ‘don’t skip more than 48 hours’? That’s not science-that’s guilt-tripping. I skipped a week because I was sick. Does that make me a failure? No. It makes me human.
Stop pretending movement is the answer. The real answer is dietary discipline. Everything else is noise.
siddharth tiwari
December 28, 2025 at 00:02ok but did u know that the ADA is funded by big pharma? they push exercise so you dont ask why your insulin costs 300 bucks?
also my cousin in delhi got his diabetes cured by drinking neem juice and doing yoga at 4am. no one talks about that. why? because they dont want you to know you dont need meds.
and why is everyone always talking about ‘glucose monitors’? who’s tracking you? are you sure your pump isnt sending data to the government?
i dont trust any of this. i walk 10 steps and my sugar spikes. so i sit. and i eat chips. and i laugh. because they cant control me.
bharath vinay
December 29, 2025 at 02:51So let me get this straight: you’re telling people to exercise to reduce insulin resistance… but you’re also telling them to lower their insulin doses? That’s a contradiction. If exercise makes you more sensitive, why do you need to reduce insulin? Unless… they’re lying about the whole thing.
And why is HIIT ‘risky’? Because it’s too effective. They don’t want you to know you can fix this without drugs. They want you dependent. That’s why they say ‘talk to your doctor’-because your doctor gets paid to keep you on insulin.
Wake up. This is all a money game. Movement is a distraction. The real cure is off the grid. And no one here wants to talk about it.
Andrea Di Candia
December 29, 2025 at 17:59Wow. I read all of this. And I still believe in walking after dinner.
To the conspiracy folks: I’m not here to sell you a pill. I’m here because my dad died of diabetic complications at 59. I don’t want that for my kids.
To the contrarians: I’ve tried fasting. I’ve tried keto. I’ve tried everything. What kept me alive was consistency-not ideology.
To the guy who said his sugar went up after walking: maybe try walking after lunch instead. Or add a little protein. Or test at a different time. Try something. Don’t quit because one experiment didn’t go your way.
We’re all just trying to survive this. Let’s not turn this into a battlefield. Let’s just move. Together.