PAMORAs like methylnaltrexone, naloxegol, and naldemedine target opioid-induced constipation without affecting pain relief. Learn how they work, who benefits most, and what to expect from treatment.
Opioid Constipation: What It Is, Why It Happens, and How to Manage It
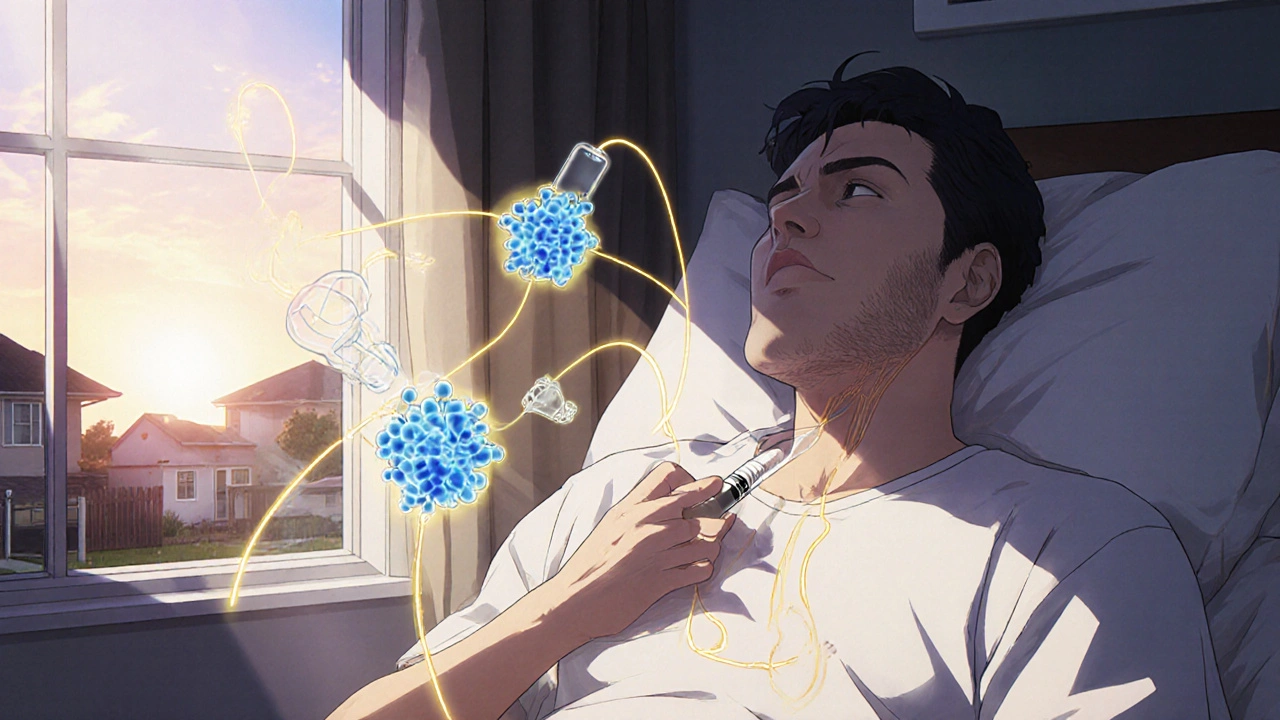
When you take opioids for pain, your body doesn’t just feel less pain—it also slows down your digestive system. This isn’t a rare side effect. It’s opioid constipation, a direct result of opioids binding to receptors in the gut that control bowel movement. Also known as opioid-induced constipation, it affects up to 90% of long-term users, and many people suffer in silence because they think it’s just normal. Unlike regular constipation from diet or dehydration, opioid constipation doesn’t get better with more water or fiber alone. The drugs literally lock your bowels in place.
This isn’t just about discomfort. Untreated opioid constipation can lead to bowel obstruction, nausea, loss of appetite, and even hospitalization. It’s also one of the top reasons people stop taking pain meds they need. bowel function, the natural rhythm of digestion and elimination gets disrupted because opioids reduce gut motility, increase fluid absorption in the intestines, and relax the muscles that push stool out. Even low doses can trigger it, and it doesn’t fade with tolerance like pain relief does.
Many people try over-the-counter laxatives, but most don’t work well for this type of constipation. Traditional stimulant laxatives might give quick relief but can cause cramping or dependency. Newer treatments like laxatives for opioid use, specifically designed to block opioid effects in the gut without reducing pain relief are available by prescription. These include drugs like methylnaltrexone and naloxegol—medications that act only in the intestines, leaving pain control untouched.
What you do daily matters too. Movement helps—even a short walk after meals. Staying hydrated is still important, even if water alone won’t fix it. Some people find relief with probiotics or magnesium, though evidence is mixed. The key is to talk to your doctor early. Don’t wait until you’re in pain or bloated for days. Your pain management plan should include a bowel plan, not just a pain plan.
What you’ll find below are real, practical guides from people who’ve dealt with this. You’ll see how others managed it without quitting their meds, what worked and what didn’t, and how to ask your doctor for the right help. No fluff. No guesswork. Just clear advice from real experiences.