Birth control pills are one of the most common ways women in the U.S. prevent pregnancy - but they’re not as simple as popping a pill every day and forgetting about it. If you’re considering them, or already using them, you need to know the real numbers: birth control pills are 99% effective only if taken perfectly. In real life? That number drops to about 93%. That means 7 out of every 100 women using the pill will get pregnant in a year - not because the pill doesn’t work, but because life happens. You forget. You’re sick. You take it late. Or you start a new medication that makes it less effective.
How Birth Control Pills Actually Work
There are two types of birth control pills: combined pills and progestin-only pills. Combined pills contain estrogen and progestin. Progestin-only pills, often called the "mini-pill," contain just progestin. Both stop ovulation - meaning your ovaries don’t release an egg. They also thicken cervical mucus so sperm can’t swim through, and thin the lining of the uterus so a fertilized egg can’t stick. Most combined pills today contain between 20 and 35 micrograms of estrogen - a far cry from the 10,000 micrograms in the first pill approved in 1960. Lower doses mean fewer side effects and less risk. The safest option for most people is a pill with 30 micrograms of ethinyl estradiol and levonorgestrel, according to the Cleveland Clinic. Progestin-only pills like Slynd® use 4 mg of drospirenone in a 24/4 cycle (24 active pills, 4 placebo), which helps reduce breakthrough bleeding.Effectiveness: Perfect Use vs. Typical Use
Here’s the hard truth: the number you see on the box - 99% effective - is based on perfect use. That means taking the pill at the exact same time every single day, without missing a single dose. In reality, most people don’t do that. Studies show that with typical use - which includes forgetting pills, taking them late, or vomiting after taking one - the failure rate jumps to 7% per year. That’s 7 pregnancies for every 100 women using the pill. Virginia Tech’s health center puts it even higher: 5% failure rate with typical use. That’s 50 pregnancies per 1,000 users. Why does this happen? Younger women - especially those under 21 - are more likely to miss doses. A 2021 JAMA review found that women under 21 using birth control pills had almost twice the risk of unintended pregnancy compared to women 21 and older. No such gap exists with IUDs or implants. Why? Because those don’t rely on daily habits. Pills demand consistency. Life gets busy. You travel. You sleep in. You forget. If you miss a pill, what do you do? Take it as soon as you remember. If it’s been more than 24 hours, use a backup method like condoms for the next 7 days. And remember: the pill doesn’t start working right away. You need to take it for 7 full days before you’re protected. Use condoms during that first week.Side Effects: What Most Women Experience
Not everyone has side effects, but many do - especially in the first 2 to 3 months. The most common ones are:- Nausea - usually goes away after a few weeks
- Breast tenderness
- Mild headaches
- Bloating
- Spotting between periods
- Changes in mood
What Medications Can Make Birth Control Pills Less Effective?
This is where people get caught off guard. Many drugs interfere with how your body processes the hormones in birth control pills. You might not realize it until it’s too late. Antibiotics: Only one - rifampin (Rifadin) - is proven to reduce effectiveness. But many doctors still advise using backup contraception when taking any antibiotic, just to be safe. Anti-seizure drugs: Phenytoin, carbamazepine, oxcarbazepine, topiramate, and phenobarbital can make the pill useless. If you take any of these, talk to your doctor about switching to an IUD or implant. HIV meds: Some antiretrovirals, like efavirenz and nevirapine, reduce hormone levels. Herbal supplements: St. John’s wort is a big one. It’s sold as a natural remedy for depression, but it speeds up how fast your liver breaks down estrogen and progestin. A 2019 study found women taking St. John’s wort with the pill had significantly higher rates of breakthrough bleeding and unintended pregnancy. Griseofulvin: An antifungal used for nail or skin infections - also reduces pill effectiveness. Always tell your doctor or pharmacist you’re on birth control pills before starting any new medication, even over-the-counter ones. And if you’re taking something that interferes, use condoms for at least 7 days after stopping it.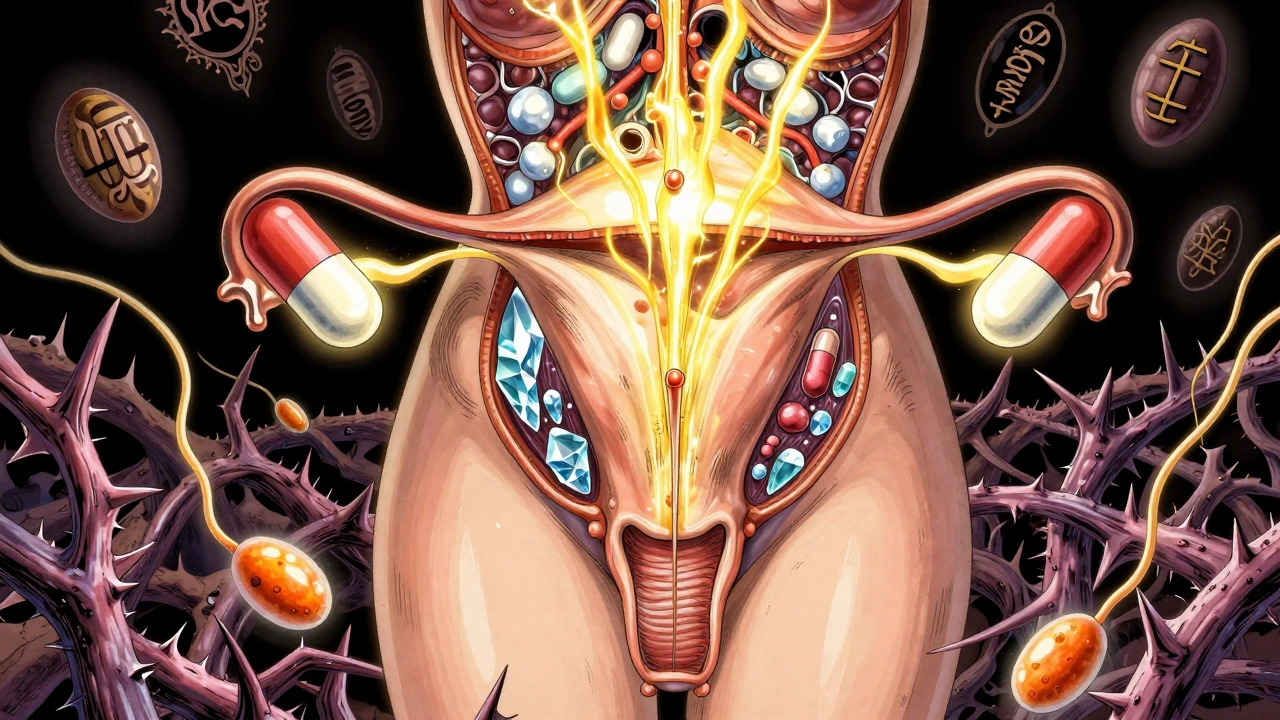
Benefits Beyond Pregnancy Prevention
Birth control pills aren’t just for avoiding pregnancy. Many women use them to manage other health issues:- Regulate periods - especially if they’re heavy, irregular, or painful
- Reduce PMS and PMDD symptoms
- Improve acne
- Lower risk of endometrial cancer by up to 50% - protection lasts up to 20 years after stopping
- Reduce ovarian cancer risk by 27% - the longer you use the pill, the greater the protection
- Lower colon cancer risk by about 18%
What Happens When You Stop Taking Them?
Some women worry they’ll be infertile after using the pill. That’s not true. A CDC study found that 97% of women had their first period again within 90 days after stopping combined pills. Fertility returns quickly. If you’re trying to get pregnant, you can start right away. No waiting period needed.How Do Pills Compare to Other Methods?
Here’s the reality check: birth control pills are the most popular reversible method in the U.S., used by about 22% of women on contraception. But they’re not the most effective.| Method | Typical Use Failure Rate | Perfect Use Failure Rate |
|---|---|---|
| Birth control pills | 7% | <1% |
| Condoms | 13% | 2% |
| Birth control patch | 7% | <1% |
| Birth control ring | 7% | <1% |
| IUD (hormonal or copper) | 0.8-2% | 0.6-1.5% |
| Implant | 0.1% | 0.1% |
| Sterilization (tubal ligation) | 0.4% | 0.2% |

Who Should Avoid Birth Control Pills?
You should not take combined birth control pills if you:- Smoke and are over 35
- Have a history of blood clots, stroke, or heart attack
- Have uncontrolled high blood pressure
- Have migraines with aura
- Have certain types of breast cancer
- Have liver disease
What If the Pill Isn’t Working for You?
If you’re having bad side effects, forgetting pills regularly, or just feel like it’s not the right fit - you’re not alone. And you don’t have to stick with it. There are better options. IUDs last 3 to 12 years. Implants work for 3 to 5 years. The patch and ring are weekly and monthly alternatives. All of these are more effective than the pill and require less daily effort. Talk to your doctor about switching. Don’t just quit cold turkey - that can cause spotting, mood swings, or even a surprise pregnancy. Your doctor can help you transition safely.Bottom Line
Birth control pills are a solid choice if you can take them every day without fail. They offer real health benefits beyond pregnancy prevention. But if your life is busy, unpredictable, or you’re under 21, you’re better off with an IUD or implant. They’re more effective, require less effort, and give you peace of mind. And always use condoms. Birth control pills don’t protect against STIs. If you’re with a new partner, or not sure about your partner’s status, condoms are non-negotiable.Can birth control pills cause weight gain?
Most studies show birth control pills don’t cause significant weight gain. Some women notice slight water retention or bloating, especially in the first few months, but this usually fades. A 2020 review of 49 studies found no consistent link between oral contraceptives and long-term weight gain. If you’re gaining weight, it’s more likely due to lifestyle, stress, or other hormones - not the pill.
Do birth control pills affect mood or cause depression?
Some women report mood changes, irritability, or sadness when starting the pill. A large Danish study of over 1 million women found a small increased risk of being prescribed antidepressants among pill users, especially teens. But correlation isn’t causation. Many factors influence mood. If you feel worse after starting the pill, talk to your doctor. Switching to a different progestin - like drospirenone or norgestimate - often helps. Don’t assume it’s "all in your head."
Can I skip my period on birth control pills?
Yes. Many women choose to skip their placebo week and go straight to the next pack. This is called continuous or extended-cycle use. It’s safe and approved by the American College of Obstetricians and Gynecologists. You might get spotting at first, but most women stop bleeding after a few months. It’s especially helpful for those with painful periods, endometriosis, or migraines triggered by hormones.
How soon after stopping the pill can I get pregnant?
You can get pregnant right away. Fertility returns quickly - often within weeks. A CDC study found 97% of women had their first period again within 90 days of stopping the pill. There’s no need to wait. If you’re trying to conceive, start tracking ovulation or using ovulation predictor kits to increase your chances.
Are generic birth control pills as good as brand-name ones?
Yes. The FDA requires generic pills to have the same active ingredients, dosage, and effectiveness as brand-name versions. The only differences are in inactive ingredients - like fillers or dyes - which rarely cause issues. Most women switch to generics without any problems. If you notice new side effects after switching, talk to your doctor. But cost savings are real - generics can be 80% cheaper.




Donna Hammond
December 12, 2025 at 20:41So many people think the pill is just ‘pop and forget’-but it’s so much more nuanced. I’ve been on it for 8 years and the biggest game-changer was switching from a 35mcg estrogen pill to a 20mcg one with drospirenone. My acne cleared up, the bloating vanished, and I actually started looking forward to my period instead of dreading it. It’s not one-size-fits-all, and your doctor should help you tweak it until it clicks.
Richard Ayres
December 14, 2025 at 00:43The data presented here is both accurate and refreshingly transparent. It's important to emphasize that the 93% typical use rate isn't a failure of the medication-it's a reflection of human behavior. When we design public health interventions, we must account for real-world constraints: sleep schedules, travel, stress, and access to consistent care. Long-acting reversible contraceptives are not just more effective-they're more equitable.
Sheldon Bird
December 14, 2025 at 03:56Y’all need to stop acting like the pill is some magical potion 😅 I’ve seen so many friends stress out over missing one pill like it’s the end of the world. Pro tip: if you’re that forgetful, get an IUD. No judgment-just real talk. My cousin switched last year and now she’s got time to focus on her art instead of her pill schedule 🎨✨
Karen Mccullouch
December 14, 2025 at 22:44They don’t want you to know this, but Big Pharma is pushing pills because they make more money off you taking them every day than if you got an implant once and forgot about it. And don’t even get me started on St. John’s Wort-some of those ‘natural’ supplements are literally designed to sabotage your birth control. Read the fine print, people. Your body isn’t a lab rat.
Michael Gardner
December 15, 2025 at 03:49Interesting how everyone treats the 7% failure rate like it’s a flaw. But if you look at it differently-7% of women get pregnant while using the pill-that’s actually a huge success rate compared to, say, condoms. Maybe the problem isn’t the pill. Maybe it’s that we’ve been sold the myth that perfect use is normal. It’s not. It’s aspirational.
Willie Onst
December 15, 2025 at 13:42Man, I wish my high school health class had talked about this stuff like real humans instead of just saying ‘use condoms’ and calling it a day. I didn’t know you could skip your period on the pill until I was 24. Or that generics were just as good. Or that the pill could help with my cramps so much. This post is the kind of info that actually saves lives-not just scares people.
Ronan Lansbury
December 17, 2025 at 12:31Let’s be honest-the entire reproductive health industry is a construct of patriarchal medicine. Why are we still relying on hormonal manipulation to control fertility when the body is a complex, self-regulating system? The pill was invented in the 1950s to control women’s bodies, not empower them. I’d rather trust my circadian rhythm than a synthetic estrogen molecule. The real revolution? Abstinence.
Jennifer Taylor
December 18, 2025 at 13:29Okay but have you heard about the NEW study that says birth control pills are linked to increased risk of breast cancer in women under 25?? I read it on a blog and it was like, ‘THEY’RE HIDING THIS FROM YOU’ and then there was a video of a woman crying in a pharmacy. I’m not saying it’s true but… what if it is?? And what about the chemicals in the packaging?? Are they leaching into the pills?? I’m scared now 😭
Shelby Ume
December 19, 2025 at 15:46As a nurse practitioner who’s prescribed birth control for over 15 years, I want to say this plainly: the pill is not a one-size-fits-all solution-and that’s okay. What matters is that you have access to accurate information, a nonjudgmental provider, and options beyond the pill. If you’re struggling with adherence, it’s not your fault. It’s a system failure. Let’s normalize switching methods. Let’s normalize asking for help. And let’s stop shaming women for needing something that works for their lives-not just their biology.