Crohn's disease and ulcerative colitis are both forms of inflammatory bowel disease, but they differ in location, depth of inflammation, complications, and treatment. Understanding these differences is key to proper diagnosis and care.
Crohn's vs UC: Key Differences, Symptoms, and Treatment Insights
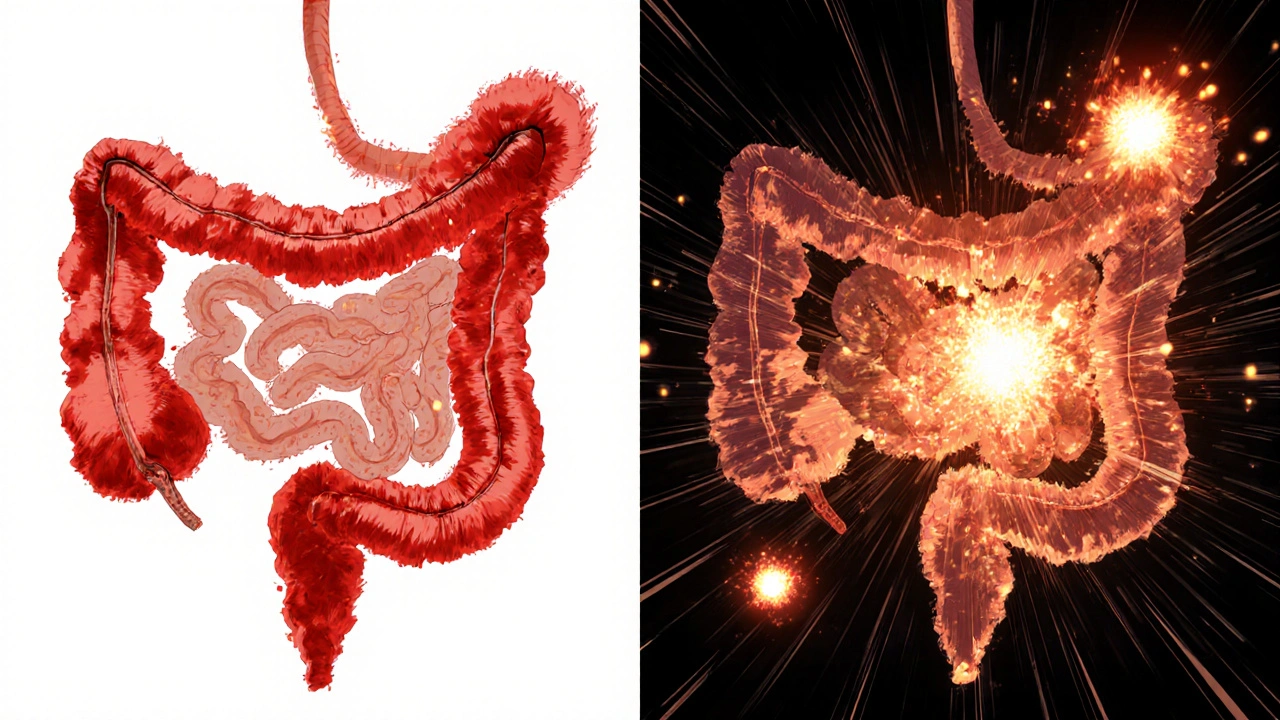
When people talk about Crohn's disease, a type of inflammatory bowel disease that can affect any part of the digestive tract and ulcerative colitis, a condition limited to the colon and rectum that causes ulcers and inflammation, they’re often referring to two sides of the same coin—inflammatory bowel disease, a group of chronic gut disorders involving immune-driven inflammation. But they’re not the same. Crohn’s can strike anywhere—from mouth to anus—and often digs deep into tissue layers. Ulcerative colitis sticks to the inner lining of the colon and starts at the rectum, spreading upward. Knowing which one you have changes everything: treatment, diet, surgery risk, and even long-term outlook.
People with Crohn’s often deal with pain anywhere in the abdomen, weight loss, and fistulas—abnormal tunnels between organs. Ulcerative colitis usually means frequent bloody diarrhea, urgency, and cramping focused in the lower left side. Neither is caused by stress or bad food, but both can flare up because of infections, meds, or immune triggers. You can have both conditions and still get misdiagnosed—many doctors start with UC because it’s easier to spot on a colonoscopy. But if biopsies show granulomas or the inflammation skips areas, that’s Crohn’s. And if your entire colon is inflamed evenly, it’s likely UC. The right diagnosis matters because drugs like vedolizumab work better for UC, while anti-TNFs like adalimumab often help Crohn’s patients more. Even surgery differs: removing the colon can cure UC, but it won’t fix Crohn’s if it’s already in the small intestine.
What you’ll find below isn’t just another list of drugs or symptoms. These are real stories from people who’ve lived with one or both conditions, paired with practical guides on managing side effects, navigating insurance for biologics, and understanding how medications like PAMORAs or diuretics can intersect with gut health. You’ll see how skin reactions from blood thinners might overlap with IBD flares, how inhaler technique isn’t just for asthma, and why knowing your out-of-pocket maximum matters when you’re paying for monthly biologics. This isn’t theory. It’s what works when you’re trying to eat, sleep, and live without being tied to a bathroom.