More than 1 in 10 people in the U.S. say they’re allergic to penicillin. But here’s the truth: 9 out of 10 of those people aren’t actually allergic. That’s not a typo. It’s a quiet public health crisis hiding in plain sight - and it’s putting your health at risk.
Why Most Penicillin Allergies Are Wrong
Penicillin was discovered in 1928, and for decades, it was the miracle drug that saved millions. But somewhere along the way, people started labeling rashes, stomach upset, or headaches as “penicillin allergies.” Many of these reactions were never true allergies - just side effects. A child gets a rash after taking amoxicillin for an ear infection? Parents assume it’s an allergy. Years later, that label sticks in medical records - even if the person hasn’t taken penicillin since they were five. The CDC confirms this: only about 1% of the population has a real penicillin allergy. Yet 10% carry the label. That mismatch means doctors avoid the safest, most effective antibiotics - not because they’re being cautious, but because they’re working with bad data. When you’re labeled allergic to penicillin, you’re often given alternatives like vancomycin, clindamycin, or broader-spectrum drugs. These aren’t just more expensive. They’re less targeted. They kill good bacteria along with bad. And that’s how you end up with C. difficile infections, MRSA, or longer hospital stays. Studies show patients with a penicillin allergy label have a 50% higher chance of getting MRSA and a 35% higher chance of C. difficile. All because the right antibiotic was avoided.What a Real Penicillin Allergy Looks Like
Not all reactions are the same. There are two main types: immediate and delayed. Immediate reactions happen within an hour. These are IgE-mediated - your immune system overreacts fast. Symptoms include hives, swelling of the lips or throat, trouble breathing, dizziness, or a sudden drop in blood pressure. This is anaphylaxis. It’s rare - but it’s life-threatening. If you’ve ever had swelling in your throat or passed out after taking penicillin, you need to be evaluated by an allergist. Delayed reactions show up hours or days later. A rash that shows up three days after taking amoxicillin? That’s common. But it’s rarely a true allergy. Most of these rashes are viral in origin - you had a cold, took the antibiotic, and the rash appeared anyway. These don’t mean you’re allergic. They just mean your body was reacting to something else. Severe delayed reactions - like Stevens-Johnson Syndrome or DRESS - are rare. But they’re serious. If you’ve had blistering skin, fever, swollen lymph nodes, or organ damage after taking penicillin, you need to avoid all beta-lactam antibiotics. But if you had a simple rash, itching, or upset stomach? You’re probably fine.Testing Is Safe - and Simple
The gold standard for checking a penicillin allergy is skin testing. It’s quick, safe, and accurate. A small amount of penicillin is placed under your skin. If you’re allergic, you’ll get a raised bump - like a mosquito bite - within 15 to 20 minutes. If the skin test is negative, you’ll usually get an oral challenge: a full dose of amoxicillin, taken under observation. You’ll be monitored for an hour. If nothing happens? You’re not allergic. That’s it. This isn’t experimental. It’s standard care. The CDC, the American Academy of Allergy, Asthma & Immunology, and major hospitals like Mayo Clinic and CHOP all use this protocol. And here’s the kicker: after a negative test, your risk of anaphylaxis drops to the same level as someone who’s never claimed an allergy. And here’s what most people don’t know: if you haven’t taken penicillin in 10 years, your allergy likely faded. Eighty percent of people who had a true IgE-mediated reaction lose their sensitivity over time. That rash you got as a kid? It probably doesn’t matter anymore.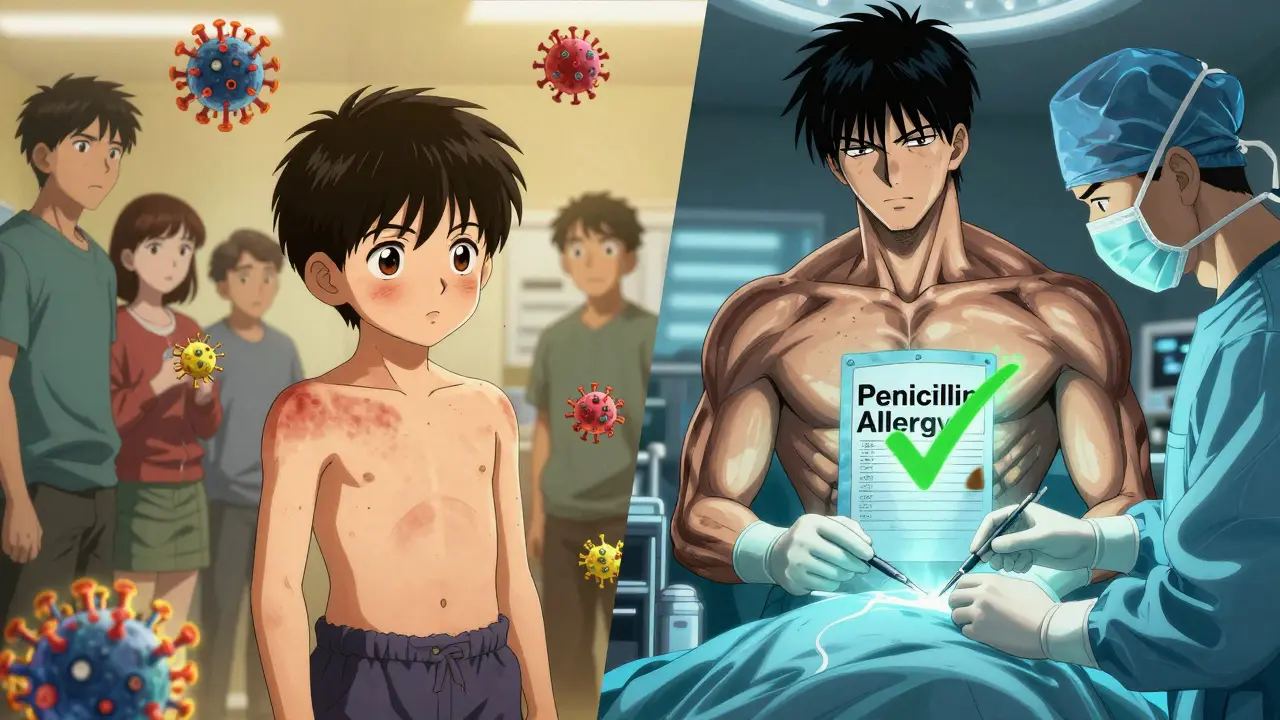
Who Should Get Tested - And Who Shouldn’t
Not everyone needs testing. But most people who think they’re allergic should consider it. Low-risk candidates: You had a rash more than five years ago. You had nausea or diarrhea. You were told you were allergic as a child, but no one ever tested you. You had itching without hives. These are all low-risk. You can likely skip the skin test and go straight to an oral challenge under supervision. Moderate-risk candidates: You had hives, swelling, or trouble breathing within five years of taking penicillin. You had a reaction during surgery or a hospital stay. You need testing before you get beta-lactam antibiotics again. High-risk candidates: You’ve had anaphylaxis, Stevens-Johnson Syndrome, or organ damage. Don’t try to test yourself. You need to see an allergist. These reactions are dangerous and require specialized care. If you’re scheduled for surgery - especially joint replacement - and you’re labeled allergic, ask your doctor: “Can I be tested before the procedure?” Cefazolin, a common antibiotic used to prevent surgical infections, is safe for 95% of people with a penicillin label - if they’ve been properly evaluated.What Happens After You’re De-Labelled
Once you’ve been cleared, the work isn’t done. You need to make sure the label is removed - from your chart, your pharmacy records, and your medical alert bracelet. Your doctor should document the test results clearly: “Penicillin allergy ruled out after negative skin test and oral amoxicillin challenge.” That note goes into your electronic health record. It should also be printed and given to you. If you wear a medical alert bracelet that says “Penicillin Allergy,” take it off. You’re not allergic anymore. Wearing that bracelet could cause a doctor to avoid the best antibiotic for you in an emergency. And tell your family. Tell your dentist. Tell your pharmacist. Mislabeling isn’t just your problem - it affects everyone who treats you.
The Bigger Picture: Why This Matters
This isn’t just about you. It’s about antibiotics we can’t afford to lose. Every time we use a broad-spectrum drug instead of penicillin, we push bacteria toward resistance. Penicillin kills the infection without wrecking your gut flora. Alternatives don’t. And when we overuse those alternatives, we create superbugs. The CDC estimates that fixing penicillin mislabeling could save the U.S. healthcare system $1.2 billion a year. That’s not just money. It’s fewer hospital stays. Fewer resistant infections. Fewer deaths. And here’s the most powerful part: you don’t need to wait for a hospital program to start. You can ask for testing now. Most allergists and primary care doctors can order it. Some pharmacies even offer penicillin allergy clinics.What to Do Next
If you’ve ever been told you’re allergic to penicillin - even if it was decades ago - here’s your action plan:- Check your medical records. Does it say “penicillin allergy” without any details?
- Ask your doctor: “Was this tested? Or was it just noted?”
- If it wasn’t tested, ask if you’re a candidate for skin testing and an oral challenge.
- If you’re low-risk, request a supervised amoxicillin challenge - it’s safe, fast, and free of risk if done right.
- Once cleared, get the results documented in writing and update your records.
- Remove any medical alert jewelry that says you’re allergic.
Can I outgrow a penicillin allergy?
Yes. About 80% of people who had a true IgE-mediated penicillin allergy lose their sensitivity after 10 years without exposure. Even if you had a serious reaction as a child, you may no longer be allergic. Testing is the only way to know for sure.
Is a rash after penicillin always an allergy?
No. Many rashes that appear after taking penicillin are caused by viruses, not the drug. If you had a rash more than five years ago, with no other symptoms like swelling or breathing trouble, it’s very unlikely to be a true allergy. Skin testing can confirm this.
Can I take cephalosporins if I’m allergic to penicillin?
Most people can. First-generation cephalosporins like cefazolin are safe for 95% of people with a penicillin label - especially if they’ve been tested. The risk of cross-reactivity is less than 1%. But if you’ve had a severe reaction like anaphylaxis or Stevens-Johnson Syndrome, you should avoid all beta-lactams until evaluated by an allergist.
What if I need an antibiotic right now and can’t wait for testing?
If you’re in an emergency or need immediate treatment, your doctor will choose an alternative like clindamycin or vancomycin. But don’t accept this as permanent. Once you’re stable, schedule testing. Avoiding penicillin long-term increases your risk of resistant infections.
Is penicillin allergy testing covered by insurance?
Yes, in most cases. Skin testing and oral challenges are covered by Medicare, Medicaid, and most private insurers in the U.S. as medically necessary procedures. Ask your doctor’s office to confirm coverage before scheduling.
Can I test myself at home?
Never. Self-testing with penicillin or amoxicillin is dangerous. Anaphylaxis can happen within minutes. Testing must be done in a medical setting with emergency equipment and trained staff on hand.
What happens if I’m still allergic after testing?
If testing confirms a true allergy, you’ll be advised to avoid all penicillin and related antibiotics. You’ll receive a written plan, including which drugs to avoid and what alternatives are safe. You may also be given an epinephrine auto-injector and advised to wear a medical alert bracelet.





Tiffany Wagner
January 24, 2026 at 03:39I got labeled allergic to penicillin when I was six after a rash from amoxicillin. Never got tested. Turned out I was fine. Now I take it like it's water. Why did no one tell me this sooner?
Chloe Hadland
January 25, 2026 at 09:19This is so important. My mom had the same thing. She avoided all antibiotics for 40 years because of a childhood rash. Then she got a bad infection and they had to use something way stronger. She cried when she found out she wasn't allergic. 😭
Amelia Williams
January 27, 2026 at 08:29Guys. This isn't just about saving money. It's about saving lives. I work in ER. We see people with C. diff because they were given vancomycin instead of amoxicillin. And half the time? They weren't even allergic. Just got a rash. And now they're in the hospital for weeks. We need to stop treating labels like facts. Get tested. It's easy. It's safe. It's free. Stop letting a childhood mistake haunt your adult health.
Viola Li
January 27, 2026 at 23:27Of course the system is broken. Big Pharma doesn't want you taking cheap penicillin. They make billions off the alternatives. The whole allergy thing is just a profit scheme disguised as safety. They'll never admit it. But you know what? I'm not buying it.
Vatsal Patel
January 28, 2026 at 14:57People think science is about facts. It's not. It's about narratives. You get labeled allergic, and suddenly your body becomes a story the system tells about you. The rash? It was never about penicillin. It was about your immune system screaming for attention. You think testing fixes that? Nah. You just get a new label. 'Non-allergic'. Still a label. Still not you.
John McGuirk
January 30, 2026 at 11:42Wait. So you're telling me the government is lying about penicillin? And the CDC? And the Mayo Clinic? All part of a plot? I mean... I know they put fluoride in the water. And 5G is mind control. So why not this? Maybe the real allergy is to being controlled by doctors. Maybe penicillin is a mind control drug. That's why they want you to take it. To keep you docile.
Michael Camilleri
January 30, 2026 at 12:52I've been saying this for years. People are too lazy to think for themselves. You get a rash? You don't research. You don't ask questions. You just let some nurse write 'penicillin allergy' in your chart and you live with it for the rest of your life. That's not an allergy. That's intellectual surrender. You're not sick. You're stupid.
lorraine england
January 31, 2026 at 06:01My dentist told me I needed an antibiotic before my root canal and I panicked because I thought I was allergic. I called my PCP and they set up a test in 2 weeks. Turned out I was fine. Best decision I ever made. Now I'm telling everyone. Seriously. If you think you're allergic, just ask. No shame. Just get it checked. You'll thank yourself later 💕
Kevin Waters
February 1, 2026 at 20:12Just had my skin test last month. Negative. Then took the amoxicillin challenge. No problem. Took me 45 minutes total. My insurance covered it. My doctor's office walked me through it. If you're scared, just go. It's not scary. It's just a tiny prick and a pill. You're not risking your life. You're reclaiming it.
Kat Peterson
February 2, 2026 at 00:48OMG I just found out I'm not allergic 😭😭😭 I've been avoiding ALL antibiotics since I was 8. My mom was so scared. I had to take Zithromax for my UTI last year and it ruined my gut. Now I'm gonna take penicillin like a queen. I'm getting a new medical bracelet that says 'Penicillin Approved' 💅💉
Himanshu Singh
February 3, 2026 at 01:44Life is like a garden. Labels are weeds. They grow because no one pulls them. But if you dig deep - if you test, if you question - you find the real soil underneath. Penicillin isn't dangerous. The fear is. Be brave. Get tested. You're not broken. You're just mislabeled. 🌱
Jamie Hooper
February 4, 2026 at 00:25so like... i had a rash after penicillin when i was a kid but i never told anyone and then i took it again last year and nothing happened. so i guess i was never allergic? idk. my doctor just shrugged. i dont even know if its in my records anymore. kinda wild how much this stuff just gets ignored lol