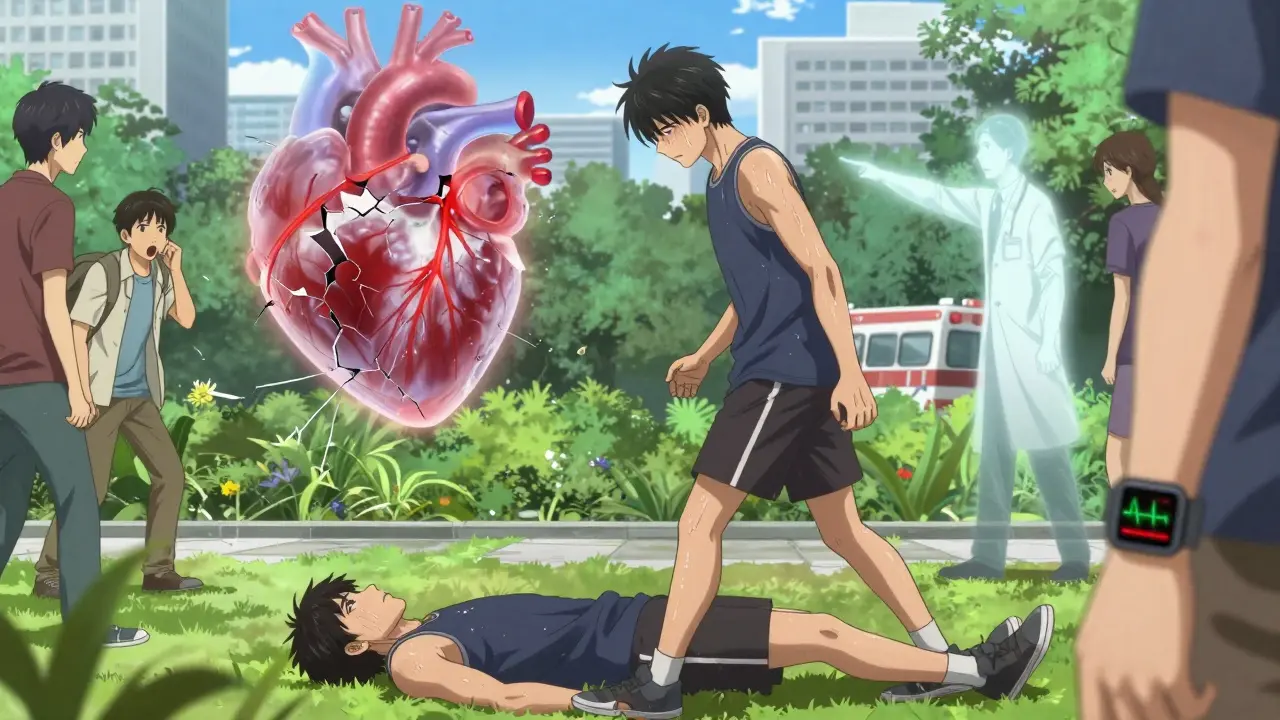
Every year, over 600,000 people in the U.S. have a heart attack. Many of them survive - but only because someone recognized the signs early and called for help. Too often, people wait. They think it’s indigestion. They blame stress. They tell themselves, It’s probably nothing. But waiting even 30 minutes can cost lives. The truth is, heart attacks don’t always look like the movies. There’s no dramatic clutching of the chest, no collapsing on the sidewalk. Sometimes, it’s just a strange pressure in your chest, or a jaw that aches for no reason. Or maybe you’re just exhausted - so tired you can’t get out of bed.
What a Heart Attack Really Feels Like
A heart attack happens when blood flow to part of your heart gets blocked. That blockage starves the heart muscle of oxygen. And without oxygen, heart cells start dying - about 1.5 million every minute. The sooner you get help, the more of your heart you save. The classic sign is chest discomfort. But it’s not always sharp pain. More often, it’s pressure. Like someone is sitting on your chest. Or a squeezing feeling. A fullness. It lasts longer than a few minutes. Or it comes and goes. You might feel it while you’re watching TV, walking the dog, or even sleeping. But here’s what most people don’t know: you don’t always feel it in your chest at all.Symptoms That Are Easy to Miss
About 65% of people have discomfort that spreads to other parts of their upper body. That means pain or pressure in your arms - especially the left one - your back, neck, jaw, or even your stomach. Some people think they have the flu. Others think it’s heartburn. A 2023 study found that 24% of heart attacks start with upper belly pain, and nearly half of those are mistaken for indigestion. Shortness of breath is another big one. It can happen with or without chest pain. You might feel winded climbing one flight of stairs, or wake up gasping for air in the middle of the night. For women, this is often the main symptom. In fact, women are 58% more likely than men to have trouble breathing during a heart attack. Other signs include:- Breaking out in a cold sweat - not from heat, not from exercise. Just suddenly, drenched in sweat.
- Nausea or vomiting - especially in women. One in four heart attack patients throws up.
- Unusual fatigue. Not just tired. Crushed tired. Women report this more than men - nearly half of women feel extreme exhaustion days or even weeks before a heart attack.
- Lightheadedness or dizziness. You might feel like you’re about to pass out.
- Palpitations. Your heart races or skips beats. It feels like it’s fluttering or pounding.
Gender Differences Matter - A Lot
Men and women can have very different heart attack experiences. About 90% of men feel chest pain. But only 64% of women do. That’s why so many women are misdiagnosed. Their symptoms don’t match the stereotype. Women are more likely to report:- Back or jaw pain without chest discomfort
- Overwhelming anxiety - like a sense of doom
- Upset stomach or nausea
- Extreme fatigue that doesn’t go away
Age Changes the Picture Too
People over 75 are more likely to have what’s called a “silent” heart attack. No chest pain. No obvious signs. Just weakness, confusion, or trouble breathing. That’s why older adults - especially those with diabetes - need to pay attention to subtle changes. A sudden loss of energy, nausea, or feeling “off” could be your body’s last warning. And it’s not just older people. Heart attacks in adults aged 25 to 44 have been rising. Younger people are getting them too. Stress, poor diet, lack of exercise, and undiagnosed high blood pressure are big factors. Don’t assume you’re too young to have one.What to Do When You Suspect a Heart Attack
If you or someone else has any of these symptoms - even if they’re mild - don’t wait. Don’t drive yourself. Don’t call a friend to come over. Don’t text your doctor. Call emergency services right away. Ambulance crews can start treatment before they even get to the hospital. They can give you oxygen, aspirin, and monitor your heart. They get you to the ER 25% faster than driving yourself. That matters. Every minute counts. If you’re not allergic to aspirin and your doctor hasn’t told you to avoid it, chew one 300mg tablet while you wait. Aspirin helps thin the blood and can reduce damage. Don’t swallow it whole - chew it. It works faster that way.Why People Wait - And Why That’s Dangerous
The average person waits three hours before calling 911. Why? Fear. Embarrassment. Denial. “I thought it was just gas.” “I didn’t want to make a fuss.” “My mom said heart attacks only happen to older men.” These are the same excuses that lead to death. One Reddit user shared how her jaw pain was diagnosed as TMJ - for two days - before she had a massive heart attack. Another man ignored chest pressure for 12 hours because he thought he’d eaten something bad. The American Heart Association found that 33% of heart attack victims wait more than two hours because they’re afraid they’re overreacting. But here’s the truth: it’s better to be wrong than dead. Emergency rooms are used to this. They see hundreds of false alarms every year. They’d rather you come in 100 times for nothing than miss one real case.
How to Prepare - Before It Happens
You can’t prevent every heart attack. But you can prepare for one.- Know your risk factors: high blood pressure, high cholesterol, diabetes, smoking, obesity, family history.
- Talk to your doctor about your risk - especially if you’re a woman over 50 or have a family history.
- Keep aspirin in your medicine cabinet. Make sure your partner, kids, or roommates know where it is.
- Teach your family the warning signs. Show them the list. Practice saying: “If I feel weird, call 911 - no excuses.”
- Consider a smartwatch with ECG. Devices like Apple Watch or Fitbit can detect irregular heart rhythms. They’re not perfect, but they can catch early warning signs.
What Happens After You Call 911
Once you’re at the hospital, they’ll run tests - EKG, blood tests for heart enzymes, maybe a CT scan. If it’s a heart attack, they’ll act fast. Some hospitals can open blocked arteries in under 90 minutes. That’s the gold standard. The goal is to restore blood flow before too much damage is done. New technology is helping. In 2023, the FDA approved an AI tool that can predict heart attacks 30 minutes before symptoms start - by analyzing EKG patterns. It’s not everywhere yet, but it’s coming. And it’s a sign that medicine is getting better at catching these events early.It’s Not Just About You
Heart attacks don’t just hurt the person having them. They hurt families. Friends. Communities. When you ignore symptoms, you risk not just your life - but the lives of everyone who depends on you. One survivor told me: “My daughter was 8 when I had my heart attack. I didn’t know I was that sick. If I’d waited another hour, I wouldn’t have seen her graduate. I wouldn’t have held my grandkids.” Don’t wait for a second opinion. Don’t wait for symptoms to get worse. Don’t wait for someone else to notice. If something feels off - your chest, your jaw, your breath, your energy - call 911. Right now. No hesitation. You might save your own life. Or someone else’s.Can you have a heart attack without chest pain?
Yes. About 36% of women and 30% of people over 75 have heart attacks without chest pain. Symptoms can include shortness of breath, nausea, jaw or back pain, extreme fatigue, or a cold sweat. These are often mistaken for other issues like indigestion or the flu, which delays treatment.
Is heart attack pain always on the left side?
No. While left arm pain is common, heart attack discomfort can radiate to either arm, the back, neck, jaw, or even the stomach. Some people feel it only in their jaw or upper back. Don’t assume it’s the left side - pay attention to any new, unexplained discomfort in your upper body.
What should I do if I think I’m having a heart attack but I’m not sure?
Call emergency services immediately. It’s better to be wrong than dead. Emergency teams are trained to handle uncertainty. They’ll run tests to confirm or rule out a heart attack. Waiting to be sure can cost your life. There’s no shame in calling - it’s the smartest thing you can do.
Can young people have heart attacks?
Yes. Heart attacks in people aged 25 to 44 have been rising since 2000. Risk factors like smoking, obesity, high blood pressure, poor diet, and stress are increasing in younger adults. Don’t assume you’re too young - if you have symptoms, take them seriously.
Should I take aspirin during a suspected heart attack?
If you’re not allergic to aspirin and your doctor hasn’t told you to avoid it, chew one 300mg tablet right away. Aspirin helps thin the blood and can reduce damage. Don’t swallow it whole - chewing it lets it enter your bloodstream faster. Only take it if you’re sure you’re not allergic. If you’re unsure, wait for emergency responders.
Can a smartwatch detect a heart attack?
No smartwatch can directly detect a heart attack. But some devices, like Apple Watch or Fitbit, can detect irregular heart rhythms such as atrial fibrillation - a condition that increases heart attack risk. If your watch alerts you to an abnormal rhythm, see your doctor. It’s not a diagnosis, but it’s a warning sign worth investigating.
Why are women’s heart attacks often misdiagnosed?
Women often have symptoms that don’t match the classic “chest pain” stereotype - like jaw pain, nausea, fatigue, or shortness of breath. Doctors, including emergency staff, are more likely to dismiss these as anxiety, indigestion, or menopause. This leads to delays. Women are 50% more likely to be sent home from the ER with a heart attack than men. Awareness and education are key to fixing this.
How long do you have to act after heart attack symptoms start?
The ideal window for treatment is 90 minutes from symptom onset. After that, heart muscle damage increases rapidly. But even if it’s been two hours, it’s still critical to get help. Every minute counts. Don’t give up - call 911 no matter how long you’ve waited.




Bryan Wolfe
January 10, 2026 at 21:56Just read this and immediately texted my mom to make sure she knows the signs - she’s 62 and keeps brushing off her jaw pain as ‘just stress.’ I’m not taking chances anymore. Seriously, if you’re reading this and you’ve ever thought ‘it’s probably nothing’ - stop. Just call 911. No shame. No embarrassment. Just life.
Prachi Chauhan
January 11, 2026 at 03:19Heart attack is not a movie. It's a whisper. A tired body saying 'help' in a language we forgot how to listen to. We think pain must scream. But sometimes it just sighs. And we ignore it because it doesn't fit the script. Maybe the real disease isn't the blocked artery - it's our denial.
Katherine Carlock
January 12, 2026 at 05:06My aunt had a silent heart attack and thought she had the flu for three days. She didn’t even have chest pain. Just... nothing. Like her body shut down slowly. She’s fine now but says she wishes she’d known this sooner. Please, share this with everyone you know. Especially your moms, grandmas, aunts - they need to know this stuff.
Sona Chandra
January 13, 2026 at 22:48WHY DO PEOPLE STILL WAIT?!?!?!?!? I had a coworker die because she waited 8 HOURS thinking it was ‘indigestion.’ She was 39. She had a kid. She had a dog. She had a life. And she thought it was ‘probably nothing.’ NO. IT WASN’T. IT WAS A HEART ATTACK. CALL 911. NOW. BEFORE IT’S TOO LATE. I’M SO ANGRY I COULD SCREAM.
Jennifer Phelps
January 14, 2026 at 16:57So if you’re over 50 and feel tired for days and your jaw aches and you’re sweating but it’s not hot what exactly do you do again? Just call 911? No tests? No second opinion? What if it’s not a heart attack? What if you waste their time? What if they laugh at you? What if you’re wrong? What if you’re right?
beth cordell
January 15, 2026 at 11:34My grandma wore a Fitbit and it flagged an irregular rhythm. She went to the doctor. Turns out she had a blocked artery. They put in a stent. She’s still here. 🙏❤️❤️❤️ I’m getting one for my dad. If it saves one life, it’s worth it. Don’t ignore the whispers. Call 911. No excuses. #HeartHealth
Lauren Warner
January 15, 2026 at 23:25Let’s be real - most people who ignore symptoms are just lazy. They don’t want to deal with the hassle. They don’t want to miss work. They don’t want to face mortality. This isn’t about ‘gender bias’ or ‘misdiagnosis’ - it’s about human cowardice. You think your discomfort is ‘just stress’? Then you deserve what happens. Stop romanticizing denial.
Craig Wright
January 16, 2026 at 14:35As a British citizen, I find it alarming that Americans delay care so long. In the NHS, we are taught from childhood that any unexplained chest discomfort warrants immediate medical attention. The notion of ‘waiting to see if it gets worse’ is not merely dangerous - it is irresponsible. I urge all readers to adopt the British standard: when in doubt, act. Now.