Colchicine-Antibiotic Safety Checker
Is Your Antibiotic Safe with Colchicine?
This tool checks if your antibiotic is safe to take with colchicine based on kidney function and drug interaction risks. Colchicine toxicity can be life-threatening when combined with certain antibiotics.
Colchicine is a simple, cheap drug. Used for over a century to treat gout, it’s now prescribed for heart conditions, pericarditis, and even some rare inflammatory diseases. But here’s the problem: if you take it with certain antibiotics-especially clarithromycin or erythromycin-you could end up in the hospital, or worse. This isn’t a rare side effect. It’s a predictable, preventable, and often missed drug interaction that kills people every year.
Why This Interaction Is So Dangerous
Colchicine doesn’t just float around in your bloodstream. It gets absorbed in your gut, pumped into your liver, and then pushed out of your cells by a transporter called P-glycoprotein (P-gp). Your liver also breaks it down using an enzyme called CYP3A4. Both systems act like safety valves. They keep colchicine levels low enough to be safe.Macrolide antibiotics like clarithromycin and erythromycin shut down both valves at once. They block CYP3A4, so your liver can’t break down colchicine. They also block P-gp, so your cells can’t push colchicine out. The result? Colchicine builds up inside your body-sometimes to five times the safe level.
The numbers don’t lie. A 2024 review in Rheumatology found that when colchicine is taken with a strong CYP3A4 inhibitor, plasma levels double. With P-gp inhibition, they can quadruple. And colchicine’s therapeutic window is razor-thin. Toxicity starts at just 3.3 ng/mL in people with kidney problems. Many patients never even know they’re at risk until they start vomiting, developing muscle pain, or seeing their blood counts crash.
Not All Macrolides Are the Same
This is where things get confusing. All macrolides look similar on paper, but their effects on your body are wildly different.- Clarithromycin: Strong inhibitor of both CYP3A4 and P-gp. This is the most dangerous combination. FDA reports show 63% of colchicine-related deaths linked to clarithromycin.
- Erythromycin: Moderate CYP3A4 inhibitor, weaker on P-gp. Still risky, but less so than clarithromycin.
- Azithromycin: Almost no inhibition of either enzyme or transporter. Safe to use with colchicine.
A 2022 study of over 12,000 patients found that those taking azithromycin with colchicine had no increased risk of toxicity. Those on clarithromycin? A 2.3-fold higher chance of severe side effects. That’s not a small difference-it’s the difference between a routine prescription and a medical emergency.
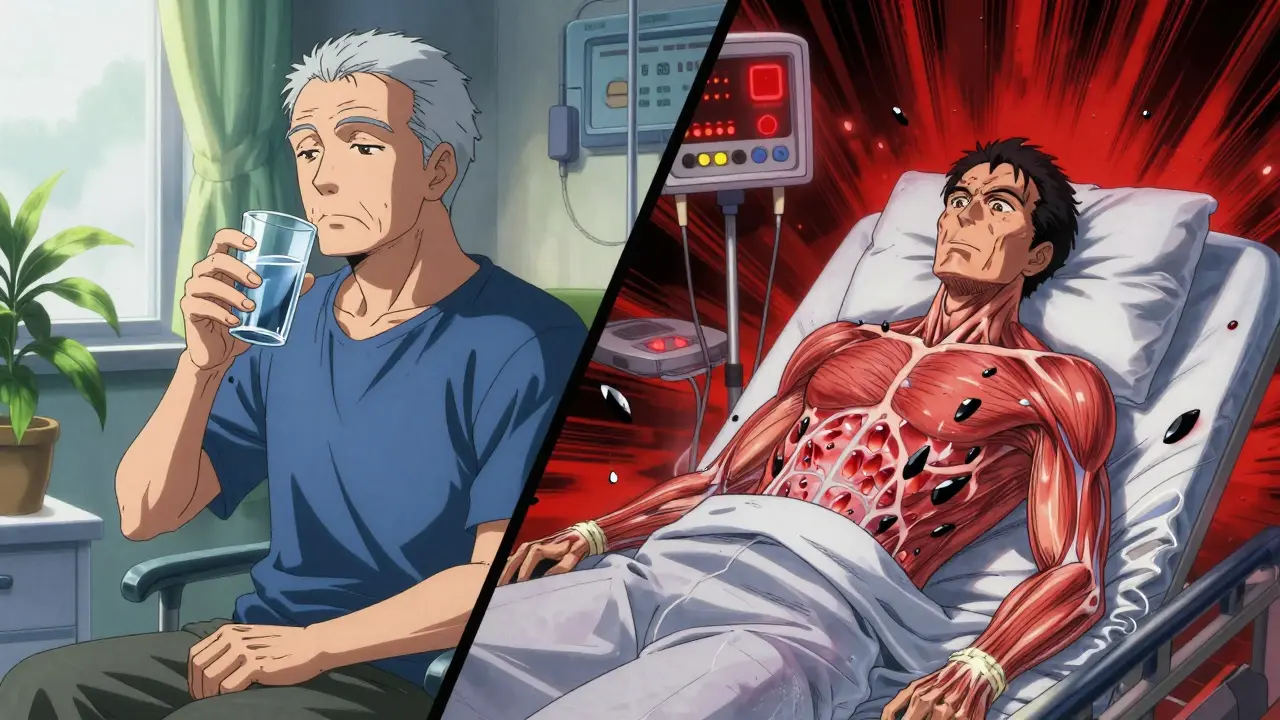
What Happens When Toxicity Strikes
Colchicine toxicity doesn’t sneak up. It hits fast and hard.Early signs: nausea, vomiting, diarrhea. These are often dismissed as stomach bugs-especially in older patients. But if they continue, things escalate. Muscle pain turns into rhabdomyolysis. White blood cell counts plummet. Bone marrow shuts down. Multi-organ failure can follow.
A 2019 case series in the Journal of Clinical Pharmacy and Therapeutics tracked 12 patients who took standard colchicine doses with clarithromycin. Three died. The rest needed ICU care. All had normal kidney function when they started. None were warned about the interaction.
Emergency room doctors see this more than you think. A 2023 survey of 245 clinicians found that 68% had treated at least one patient with this interaction. Emergency physicians reported it twice as often as rheumatologists. Why? Because the patients show up in the ER, not the clinic. And by then, it’s often too late.
Why Doctors Miss It
You’d think this would be obvious. But it’s not.Electronic health records often don’t flag it. Even when they do, the alerts are buried under dozens of other warnings. A 2024 JAMA Internal Medicine study showed that after Epic updated its alert system to prioritize high-risk interactions, inappropriate prescribing dropped by 63%. Before that? Most doctors just clicked through.
Patients don’t always tell their doctors about over-the-counter supplements. Things like St. John’s wort, grapefruit juice, or even certain herbal teas can also inhibit CYP3A4. Add those to a macrolide and colchicine, and you’ve got a perfect storm.
And here’s the kicker: many doctors still think only strong CYP3A4 inhibitors matter. But research from Hansten (2022) shows that P-gp inhibition alone can be enough to cause toxicity-especially when both systems are blocked. That’s why drugs like verapamil and diltiazem, used for blood pressure, are just as dangerous as clarithromycin.
What You Should Do If You’re on Colchicine
If you’re taking colchicine for gout, heart disease, or anything else, here’s what you need to do right now:- Check your antibiotics. If your doctor prescribes clarithromycin or erythromycin, ask: “Can I take azithromycin instead?” It works just as well for most infections and won’t interact.
- Don’t assume “low dose” is safe. Even 0.6 mg daily can be deadly if combined with a strong inhibitor. Dose reduction doesn’t eliminate risk-it just delays it.
- Know your kidney function. If your eGFR is below 60, you’re at higher risk. Colchicine clearance drops sharply with kidney impairment.
- Review all your meds. This includes supplements, antifungals (like ketoconazole), heart meds (like amiodarone), and even some HIV drugs. The list of dangerous combinations is long.
- Ask for a blood test. Colchicine levels can be measured. Only 37% of U.S. hospitals offer it, but if you’re high-risk, insist. Target levels should stay under 2.5 ng/mL.

The Bigger Picture
Colchicine isn’t going away. It’s too cheap, too effective, and too widely used. Since 2010, prescriptions have jumped 217%. Meanwhile, macrolides are still among the most prescribed antibiotics in the U.S.-around 55 million annually.That means over a million people each year are getting this dangerous combo. And most don’t know it.
Some drug companies are trying to fix this. Takeda is testing a new version of colchicine-COL-098-that doesn’t interact with P-gp. Early results show a 92% drop in interaction risk. But it’s still in trials. For now, the only solution is awareness.
There’s also a genetic angle. A 2023 Nature Medicine study found that people with two specific gene variants-CYP3A5*3/*3 and ABCB1 3435C>T-were 78% more likely to develop toxicity. These aren’t rare mutations. They’re common in people of European descent. If you’ve had a bad reaction to colchicine before, genetic testing might be worth considering.
Bottom Line
Colchicine is a powerful tool. But it’s also a landmine if you don’t know where to step.Don’t let a simple infection treatment undo months of heart protection. Don’t assume your doctor knows every interaction. Don’t wait for symptoms to appear. Ask the questions. Demand alternatives. Your life might depend on it.
Can I take azithromycin with colchicine?
Yes. Azithromycin does not significantly inhibit CYP3A4 or P-gp, making it the safest macrolide to use with colchicine. Multiple studies, including a 2022 cohort of over 12,000 patients, show no increased risk of toxicity when these two are combined. If you need an antibiotic while on colchicine, azithromycin is the preferred choice.
Is clarithromycin ever safe with colchicine?
No. Clarithromycin is a strong dual inhibitor of both CYP3A4 and P-gp, and the FDA issued a black box warning in 2010 specifically against this combination. Even with dose reduction, the risk remains unacceptably high. Clinical guidelines from the American College of Rheumatology and the American College of Cardiology explicitly recommend avoiding clarithromycin entirely in patients taking colchicine.
What if I accidentally took both drugs?
Stop the macrolide immediately. Contact your doctor or go to the ER. Symptoms of colchicine toxicity-vomiting, diarrhea, muscle weakness, unusual bruising, or fatigue-can appear within hours. Blood tests for white cell count, kidney function, and creatine kinase are critical. Colchicine levels can be measured, but treatment is mostly supportive: fluids, monitoring, and sometimes activated charcoal if ingestion was recent.
Are there other drugs besides macrolides that interact with colchicine?
Yes. Many drugs inhibit CYP3A4 or P-gp. These include: verapamil, diltiazem, itraconazole, ketoconazole, ritonavir, cyclosporine, amiodarone, and even some statins like simvastatin. Grapefruit juice is also a known inhibitor. Always review your full medication list-including supplements-with your pharmacist or doctor before starting colchicine.
Can I reduce the colchicine dose to make it safer?
For moderate inhibitors (like erythromycin or fluconazole), guidelines recommend cutting the colchicine dose by 50%. But for strong inhibitors like clarithromycin, dose reduction is not enough. The interaction is too potent. Avoidance is the only safe strategy. Even with reduced doses, toxicity has been reported in multiple case studies.
Why don’t pharmacies warn me about this?
Many pharmacy systems still don’t prioritize this interaction. A 2022 survey found that only 42% of U.S. pharmacies had automated alerts for colchicine-macrolide combinations. Even when alerts exist, they’re often overridden because they’re not specific enough. Patients need to be their own advocates. Always ask your pharmacist: “Is it safe to take this with my colchicine?”


Sally Denham-Vaughan
December 31, 2025 at 21:05My grandma was on colchicine for gout and got prescribed clarithromycin for a sinus infection. She ended up in the ER with muscle pain and vomiting. No one warned her. No one warned the pharmacist. It’s wild how common this is and how little people know. I’m telling everyone I know now.
Bill Medley
January 2, 2026 at 01:25Clarithromycin and colchicine are contraindicated per FDA and ACC guidelines. Azithromycin is the appropriate alternative. This interaction is well-documented and should be treated as a clinical emergency upon recognition.
Richard Thomas
January 3, 2026 at 17:21It’s fascinating how a molecule that’s been used for over a century can still hold such silent, deadly complexity. We think of medicine as linear-take pill A, get result B-but biology is a web. Colchicine isn’t dangerous by itself. It’s the silence between the systems-CYP3A4, P-gp, renal clearance-that lets the poison build. We’ve optimized for efficacy, not for vulnerability. And now we’re paying for it in ICU beds and obituaries. We don’t need more drugs. We need more humility in how we prescribe them.
Paul Ong
January 3, 2026 at 19:42Always ask your doc about azithromycin instead
Don’t assume low dose is safe
Check your supplements too
Your life matters more than the prescription
Andy Heinlein
January 4, 2026 at 02:00Just had my doc switch me from clarithromycin to azithromycin after I mentioned I was on colchicine. He didn’t even know the risk. I’m so glad I asked. Everyone should read this post. Seriously. Save someone’s life today. #colchicinesafety
Ann Romine
January 4, 2026 at 04:53In my country, people often use herbal teas for inflammation. I’ve seen elderly patients drink grapefruit juice daily with their colchicine. No one connects the dots. This post should be translated and shared in community centers. Awareness isn’t just medical-it’s cultural.
Todd Nickel
January 4, 2026 at 17:41There’s an underlying systemic failure here beyond individual prescribing errors. The EHR alert fatigue problem is real, but it’s symptomatic of a larger issue: drug interaction databases are built on binary flags, not probabilistic risk modeling. A patient on colchicine, verapamil, and a statin with mild renal impairment isn’t just ‘at risk’-they’re statistically overdue for toxicity. We need pharmacokinetic risk scores integrated into clinical decision support, not just ‘high-risk’ checkboxes that get ignored. The Hansten 2022 paper on P-gp alone being sufficient for toxicity is a game-changer, yet it hasn’t been incorporated into most pharmacy systems. This isn’t negligence-it’s infrastructure failure.
Austin Mac-Anabraba
January 6, 2026 at 10:21Let’s be honest. Most patients on colchicine are elderly, overweight, and on ten other meds. They don’t read the pamphlets. They trust their doctor. And most doctors are overworked, underpaid, and trained to treat symptoms, not systems. So yes, this interaction kills people. But it’s not the drugs’ fault. It’s the fault of a healthcare system that treats patients like data points and prescribes like a bingo card. Blaming clarithromycin is like blaming a hammer for broken fingers. The real problem? We stopped teaching pharmacology in medical school and started teaching billing codes.