Black Box Warning Checker
Check Your Medication Safety
Enter your prescription drug name to see if it has an FDA black box warning. This tool helps you understand the specific risks and monitoring requirements.
Result will appear here
Enter a drug name above to check for black box warnings
When you pick up a prescription, you might not notice the thick black border around a paragraph on the drug’s label. But that box? It’s the FDA’s loudest possible warning: this drug can kill you.
What Exactly Is a Black Box Warning?
A black box warning is the strongest safety alert the U.S. Food and Drug Administration can require on a prescription drug. It’s not a suggestion. It’s not a footnote. It’s a bold, black-bordered warning printed right at the start of the drug’s official prescribing information - the document doctors and pharmacists use to understand how to safely use the medicine. These warnings exist because some drugs carry risks so severe they can lead to death or permanent harm. Think: heart failure, liver damage, suicidal behavior, life-threatening infections, or sudden death. The FDA doesn’t slap this label on lightly. It’s reserved for situations where the danger is real, documented, and significant enough that the benefits might not outweigh the risks for everyone. As of 2025, more than 400 prescription medications in the U.S. carry a black box warning. That’s not a small number. It means nearly one in five commonly prescribed drugs has a risk so serious it demands this level of attention.Why Does the FDA Use a Black Box?
The FDA didn’t just pick a black border randomly. The design is intentional. It’s meant to stop you in your tracks. Unlike smaller warnings like “may cause dizziness” or “avoid alcohol,” the black box is impossible to miss. It’s formatted under strict rules (21 CFR 201.56) to stand out visually and be placed right after the most critical summary information. The goal? To force prescribers and patients to pause. To ask: “Is this really right for me?” These warnings typically cover one or more of these scenarios:- A side effect that can cause death or serious injury
- A group of people who should never take the drug (like pregnant women, people with certain heart conditions, or those with a history of depression)
- A need for strict monitoring - like monthly blood tests or frequent doctor visits
- A dangerous interaction with another drug or medical condition
How Does the FDA Decide to Add a Black Box Warning?
You might assume these warnings are added before a drug hits the market. But that’s not how it usually works. Most black box warnings are added after the drug is already being used by thousands - or millions - of patients. That’s because some risks only show up when a drug is used in the real world, not in controlled clinical trials. The FDA watches for patterns through its FDA Adverse Event Reporting System (FAERS). Doctors, pharmacists, patients, and drug companies report side effects. The system collects about 1.3 million reports a year. When a pattern emerges - say, 50 people on the same drug developed liver failure within six months - the FDA investigates. If the evidence is strong enough, the agency can require the manufacturer to add the black box. Sometimes, they’ll even demand a Risk Evaluation and Mitigation Strategy (REMS), which adds extra layers like mandatory doctor training, patient registries, or restricted distribution. Take the case of rosiglitazone (Avandia). After reports linked it to heart attacks, the FDA added a black box in 2007. Prescriptions dropped by 70% in two years. But even then, millions of patients kept taking it - because for some, the benefits still outweighed the risks.
Does a Black Box Mean You Can’t Take the Drug?
No. And this is where people get confused. A black box warning doesn’t mean “never use this drug.” It means “use this drug with extreme caution, and only if the benefits clearly outweigh the risks.” For many patients, there are no good alternatives. Someone with treatment-resistant depression might have only one drug that works - even if it carries a black box warning about suicide risk. A person with advanced rheumatoid arthritis might need a biologic that increases infection risk, because nothing else controls their pain. As Dr. Meghan Lehmann from the Cleveland Clinic says: “Having a black box warning doesn’t mean you shouldn’t take the medication. It means you need to understand the risk - and make sure your doctor is monitoring you closely.” The key is informed choice. Your doctor should sit down with you and explain:- What the specific risk is
- How likely it is to happen
- What signs to watch for
- What tests or check-ups you’ll need
- What other options exist
What Should You Do If Your Medication Has a Black Box Warning?
If you’re taking a drug with a black box warning, here’s what to do:- Read the warning. Don’t just trust your memory. Look at the printed leaflet or ask your pharmacist for the official prescribing information.
- Ask your doctor: “What’s the exact risk? How often does it happen? What symptoms should I call you about immediately?”
- Know your monitoring plan. Will you need blood tests? EKGs? Liver function checks? How often? Write it down.
- Report side effects. If you feel something’s wrong - even if it seems minor - report it to your doctor and through the FDA’s MedWatch program. Your report could help save someone else’s life.
- Don’t stop cold turkey. Some drugs with black box warnings (like antidepressants or steroids) can cause dangerous withdrawal if stopped suddenly. Always talk to your doctor first.
Are These Warnings Effective?
Yes - but not perfectly. Studies show black box warnings change prescribing habits. After the warning for rosiglitazone, doctors cut prescriptions dramatically. But the same study found that when a similar warning was issued for pioglitazone (Actos), prescriptions didn’t drop as much - because the media didn’t cover it as heavily. That tells us: awareness matters. The problem? Many patients never see the warning. They get their pill bottle, swallow the pill, and never read the fine print. Even some doctors don’t fully internalize the risks. The FDA is trying to fix this. Since 2021, they’ve required black box warnings to appear right after the “Highlights of Prescribing Information” section - making them harder to skip. They’ve also improved online access through Drugs@FDA, where you can search any drug and instantly see its warnings.What’s Next for Black Box Warnings?
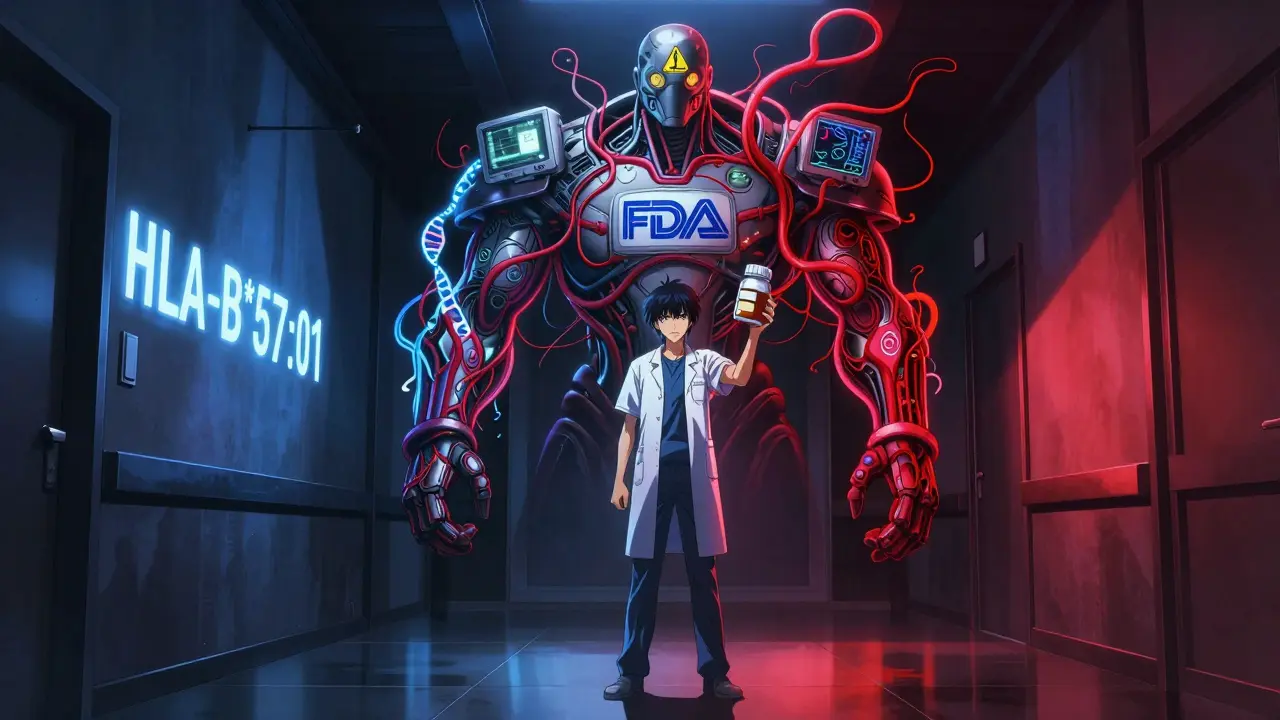
The future is getting more personal. The FDA’s 2023-2027 plan includes using genetic data to make black box warnings smarter. Instead of saying “this drug can cause liver damage in anyone,” future warnings might say: “This drug can cause liver damage in people with the HLA-B*57:01 gene variant.” That’s precision medicine. It means fewer people get unnecessarily scared - and more people who are truly at risk get protected. Digital tools are also coming. Imagine your doctor’s electronic system popping up a warning the moment they try to prescribe a black box drug - and asking them to confirm they’ve discussed the risks with you.Bottom Line: Respect, Don’t Fear
Black box warnings aren’t designed to scare you off medicine. They’re designed to make sure you and your doctor make the right call - with your eyes wide open. If you’re prescribed a drug with a black box warning, don’t panic. Don’t assume it’s dangerous for you. Ask the right questions. Understand the monitoring plan. And don’t be afraid to seek a second opinion. Because sometimes, the safest choice isn’t avoiding the drug - it’s using it wisely, with full awareness of the stakes.Do all drugs with black box warnings cause death?
No. A black box warning means the drug has the potential to cause death or serious harm in some people - not that it will. Many people take these medications safely for years. The warning exists because the risk is real enough that it must be clearly communicated. For example, birth control pills carry a black box warning for blood clots, but the actual risk for healthy women is less than 1 in 1,000 per year.
Can a black box warning be removed?
Yes. If new evidence shows the risk is lower than originally thought - or if better safety measures reduce the danger - the FDA can remove or modify the warning. This usually requires years of post-marketing data. For example, the black box warning on the antidepressant fluoxetine was updated after more data showed the suicide risk was mainly limited to teens and young adults, not all users.
Are over-the-counter drugs ever given black box warnings?
Rarely. Black box warnings are almost always reserved for prescription drugs because they require medical supervision. However, a few OTC drugs have been pulled from the market entirely due to serious risks - like phenylpropanolamine, which was removed in 2000 after linked to strokes. The FDA doesn’t use black boxes on OTC meds, but it can ban them outright if the risk is too high.
How do I check if my medication has a black box warning?
You can search the FDA’s Drugs@FDA database at fda.gov/drugsatfda. Type in the drug name - brand or generic - and click on the “Labeling” link. The black box warning will appear in the “Warnings and Precautions” section. You can also ask your pharmacist to show you the official prescribing information sheet that comes with the drug.
If I’m on a drug with a black box warning, should I avoid it during pregnancy?
It depends. Some black box warnings specifically say the drug is contraindicated in pregnancy - like isotretinoin (Accutane), which causes severe birth defects. Others, like certain antiretrovirals for HIV, are actually recommended during pregnancy because the risk of untreated disease is greater than the drug’s risk. Never assume. Always talk to your doctor before making any changes.




Retha Dungga
December 30, 2025 at 19:38Life is a risk bro 🌪️ I mean yeah black box = danger but so is crossing the street or eating avocado toast. We’re all just meat suits trying not to die while scrolling. 🤷♀️✨
Urvi Patel
January 1, 2026 at 06:23Most people don’t even read the label. The FDA’s black box is a bandaid on a bullet wound. Real solution? Ban the drugs that kill. Not just slap a warning and call it progress. Pharma’s laughing all the way to the bank.
Joy Nickles
January 1, 2026 at 17:21I had to take that antidepressant with the black box... and honestly? My therapist said if I didn't take it, I'd be dead by now. So yeah, the risk is real... but so is the alternative. I check in every week. I got bloodwork. I text my mom if I feel weird. It's not magic. It's management. 🤕💊
Robb Rice
January 2, 2026 at 06:16It's worth noting that black box warnings are not a reflection of drug quality but of risk-benefit analysis. Many life-saving medications carry them. The key is informed consent and vigilant monitoring. This is medicine, not a lottery.
Harriet Hollingsworth
January 2, 2026 at 12:00People just swallow pills like candy. You don’t read the fine print? You deserve what you get. I saw a guy on TikTok say he took 3 pills of that diabetes drug because he ‘felt tired.’ I swear to god, we’re evolving backward.
Bennett Ryynanen
January 3, 2026 at 02:41Look I get it. Black box = scary. But if your doctor says this is your best shot and you’ve tried everything else? Don’t let fear stop you. I’m alive today because I didn’t run from my meds. I leaned in. You can too. You’re stronger than you think.
Chandreson Chandreas
January 4, 2026 at 08:38The universe doesn’t care if you’re scared. It just wants you to be aware. 🌌 Black box? It’s not a death sentence. It’s a compass. Follow it. Talk to your doc. Sleep well. Drink water. And breathe. You got this.
Darren Pearson
January 5, 2026 at 00:41The FDA’s approach remains fundamentally reactive rather than proactive. One cannot help but observe the systemic failure in pharmaceutical oversight when life-altering adverse events emerge only after millions of exposures. The regulatory framework is archaic.
Stewart Smith
January 5, 2026 at 08:39So you’re telling me the same people who panic over GMOs and 5G are cool with taking a drug that could kill them... but only if it’s got a black box? Classic.
Jenny Salmingo
January 5, 2026 at 18:39My grandma took a black box drug for 12 years. Never had an issue. She said, 'I trust my doctor, and I trust my body.' Simple. But true.
Aaron Bales
January 6, 2026 at 06:35If you're on a black box drug, ask your doctor: What’s the actual risk percentage? Most people think it’s 50% when it’s 0.5%. Knowledge reduces fear.
Lawver Stanton
January 7, 2026 at 01:56I read the entire prescribing info for my ADHD med. It’s like a horror novel. 3 pages of 'can cause sudden death, psychosis, hallucinations, suicidal ideation, liver failure, and spontaneous combustion' (okay not that last one). But I’ve been on it for 7 years and I’m literally the most functional version of myself. So yeah, the warning is real. But so is the relief. It’s not black and white. It’s a messy, terrifying, beautiful gray.
Sara Stinnett
January 7, 2026 at 02:38The FDA is a puppet of Big Pharma. Black box warnings are PR tools to absolve corporations of liability. If these drugs were truly dangerous, they’d be banned-not labeled and sold for $1,200 a month. Wake up. This isn’t safety. It’s capitalism with a warning sticker.