If you’re taking apixaban for atrial fibrillation, deep vein thrombosis, or after hip or knee surgery, you’ve probably been told to watch for signs of bleeding-bruising, nosebleeds, or dark stools. But there’s another warning sign that doesn’t get enough attention: skin reactions.
What Do Apixaban Skin Reactions Look Like?
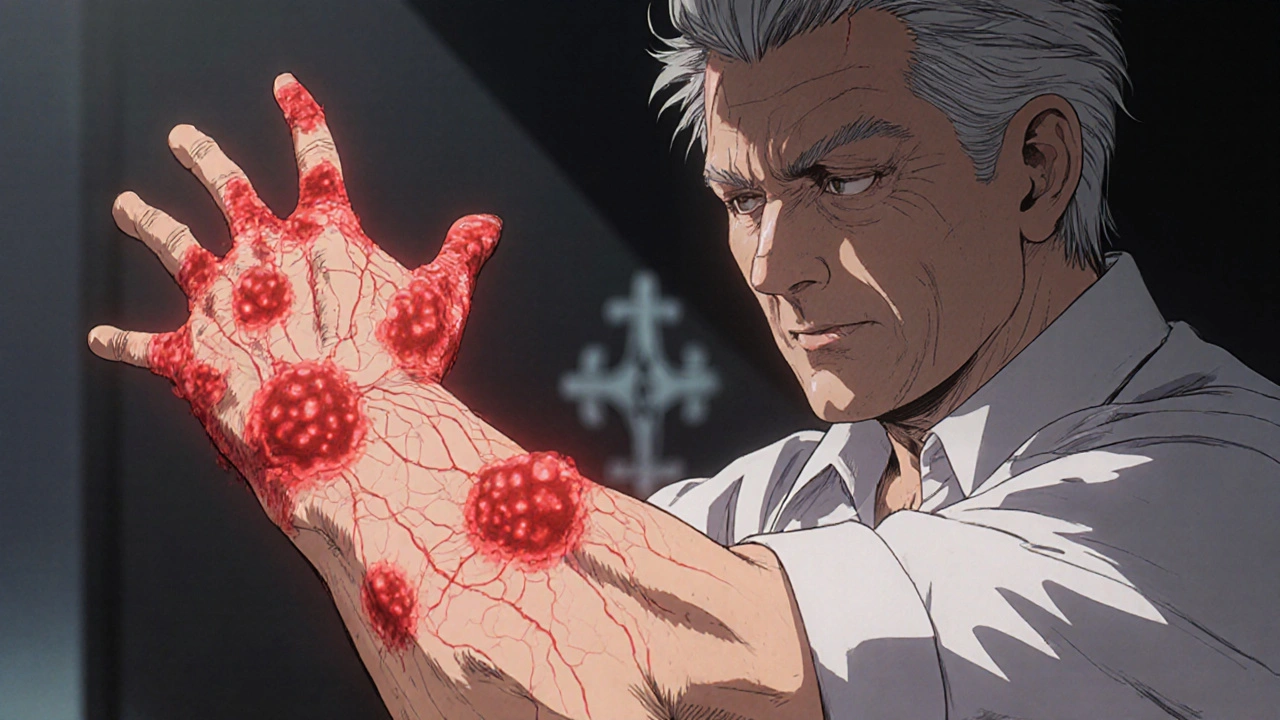
Most people on apixaban never have skin issues. But for some, the first sign something’s wrong isn’t a bruise-it’s a rash. These reactions can show up anywhere from a few days to several months after starting the drug. They’re not always obvious. You might notice:
- Red, itchy patches that don’t fade when you press on them
- Small bumps or hives that come and go
- Flaking, peeling, or dry skin that feels tight or tender
- Dark purple or reddish spots that look like bruises but aren’t from an injury
These aren’t just annoying-they can be early warnings. In rare cases, apixaban can trigger a serious condition called drug-induced hypersensitivity syndrome, which includes skin rash, fever, swollen lymph nodes, and organ inflammation. If you develop a rash along with fever, swollen glands, or trouble breathing, stop taking apixaban and get medical help immediately.
Why Does Apixaban Cause Skin Reactions?
Apixaban doesn’t directly irritate the skin. The problem is your immune system. In a small number of people, the body mistakes apixaban for a threat and starts attacking it. This triggers inflammation, which shows up as redness, itching, or swelling. It’s not an allergy in the classic sense-like a peanut reaction-but it’s still an immune response.
Studies from the U.S. Food and Drug Administration’s adverse event database show that skin-related side effects from apixaban are reported in about 1 to 3 out of every 100 users. That’s low, but it’s more common than you’d think compared to older blood thinners like warfarin. One 2023 analysis of over 12,000 patients found that 2.4% developed some form of skin reaction within the first six months of starting apixaban.
What increases your risk? You’re more likely to see a reaction if you:
- Have a history of drug rashes or allergic reactions to other medications
- Are over 75 years old
- Have kidney problems (apixaban is cleared through the kidneys)
- Take other drugs that can affect your immune system or skin, like NSAIDs or certain antibiotics
Differentiating Apixaban Reactions From Other Causes
Not every rash means apixaban is the culprit. Other possibilities include:
- Viral infections like shingles or chickenpox
- Heat rash or contact dermatitis from laundry detergent or lotions
- Psoriasis or eczema flare-ups
- Reactions to other medications you’ve started recently
Here’s how to tell the difference:
| Feature | Apixaban Reaction | Viral Rash | Contact Dermatitis |
|---|---|---|---|
| Onset | Days to weeks after starting apixaban | Usually after fever or cold symptoms | Hours to days after contact with irritant |
| Itching | Moderate to severe | Mild or none | Very intense |
| Location | Widespread, often symmetric | Follows nerve paths (shingles) or trunk/face | Localized to contact area (e.g., wrist, neck) |
| Other symptoms | Fever, fatigue, joint pain possible | Fever, sore throat, swollen glands | Only skin symptoms |
| Response to stopping apixaban | Improves within days | No change | No change |
If you’re unsure, don’t guess. Take a photo of the rash and show it to your doctor. They may check your blood counts, liver and kidney function, or even do a skin biopsy if the reaction is severe or persistent.

What to Do If You Notice a Skin Reaction
Don’t panic. But don’t ignore it either. Here’s what to do step by step:
- Take a photo. Document the rash’s size, color, and location. This helps your doctor track changes.
- Check for other symptoms. Fever? Swelling? Trouble breathing? Dizziness? If yes, go to the ER. These could signal a dangerous systemic reaction.
- Don’t stop apixaban on your own. Stopping suddenly increases your risk of stroke or blood clots. Talk to your doctor first.
- Call your prescriber. Even if the rash seems mild, they need to know. They may suggest switching to another anticoagulant like rivaroxaban or dabigatran.
- Keep a symptom log. Note when the rash appears, what you ate, what new products you used, and whether it gets worse after taking your dose.
Most mild reactions improve within a week or two after switching medications. In one 2024 study of patients who developed skin rashes on apixaban, 89% saw full resolution after switching to a different direct oral anticoagulant (DOAC), with no recurrence.
Alternatives If Apixaban Causes Skin Issues
If your skin reaction is confirmed to be linked to apixaban, your doctor will likely switch you to another DOAC. Here’s how they compare:
- Rivaroxaban - Similar to apixaban, but slightly more likely to cause gastrointestinal side effects. Skin reactions are rare but possible.
- Dabigatran - Taken twice daily. Less likely to cause skin issues, but can cause stomach upset or bloating.
- Edoxaban - Once daily, low risk of skin reactions. Often chosen for patients with kidney issues.
- Warfarin - Requires regular blood tests. Skin reactions are extremely rare, but the need for monitoring makes it less convenient.
Your doctor will pick based on your kidney function, other medications, and whether you’ve had reactions to any of these before. Most patients tolerate the switch well.

When to Be Concerned: Red Flags
Most skin reactions to apixaban are mild. But some need emergency care. Seek help immediately if you have:
- Blistering or peeling skin (like a bad sunburn)
- Sores in your mouth, eyes, or genitals
- High fever over 38.5°C (101.3°F)
- Swelling of the face, lips, or throat
- Difficulty breathing or rapid heartbeat
These could signal Stevens-Johnson syndrome or toxic epidermal necrolysis-rare but life-threatening conditions. They’re more common with certain antibiotics or seizure medications, but they’ve been reported with apixaban too. If you see any of these, go to the hospital right away.
Long-Term Outlook
If you’ve had a skin reaction to apixaban, you’ll likely be advised to avoid it-and possibly other similar drugs-forever. Re-exposing yourself to apixaban after a reaction can cause a much worse response next time.
But here’s the good news: you don’t need to go back to warfarin. Modern alternatives like dabigatran or edoxaban are just as effective at preventing strokes and clots, with fewer bleeding risks and no skin issues for most people. Many patients report feeling more confident once they’re on a medication that doesn’t cause rashes or itching.
Keep in mind: skin reactions don’t mean apixaban is unsafe for everyone. For most, it’s a reliable, well-tolerated drug. But if your skin is sending you a signal, listen. It might be the only warning you get before something worse happens.
Can apixaban cause a rash even after months of use?
Yes. While most skin reactions happen within the first few weeks, some people develop rashes after months or even years of taking apixaban. This is less common, but it’s been documented in medical case reports. If you suddenly get a new rash while on apixaban-even after a year-don’t assume it’s unrelated. Always check with your doctor.
Is a skin reaction to apixaban an allergy?
Not exactly. True allergies involve IgE antibodies and usually cause immediate reactions like hives or anaphylaxis. Apixaban reactions are more often delayed-type immune responses, similar to reactions seen with some antibiotics. You won’t test positive on a standard allergy skin test, but your immune system is still reacting to the drug.
Can I use antihistamines or steroid creams for the rash?
Mild itching can be eased with over-the-counter antihistamines like cetirizine or topical hydrocortisone cream. But these only treat the symptom, not the cause. If the rash doesn’t improve within a few days-or gets worse-you still need to talk to your doctor about switching medications. Don’t rely on creams alone.
Will I have to take blood thinners for life if I can’t take apixaban?
If you’re on apixaban for a long-term condition like atrial fibrillation, yes-you’ll need another anticoagulant. But you have several safe, effective options. Most people switch successfully to dabigatran, rivaroxaban, or edoxaban without further skin issues. Your doctor will choose based on your health profile and past reactions.
Can I take apixaban again if the rash went away?
No. Once you’ve had a confirmed skin reaction to apixaban, you should avoid it permanently. Re-exposure can lead to a much more severe reaction, including life-threatening conditions. Even if the rash seemed mild, your immune system remembers the drug. Don’t risk it.


Alex Harrison
November 5, 2025 at 23:53i started apixaban last year and got this weird rash on my arms outta nowhere. thought it was laundry detergent till i read this. never even considered the med. thanks for pointing this out, really helpful
Jay Wallace
November 6, 2025 at 09:44Of course, the FDA doesn't warn you about this-because they're too busy protecting Big Pharma. I've seen this before. Rashes? That's just the tip of the iceberg. Apixaban's a chemical abomination disguised as medicine. We need real transparency, not this watered-down fluff.
Alyssa Fisher
November 6, 2025 at 15:47It's fascinating how the body can turn a therapeutic agent into a target. The immune system doesn't distinguish between 'good' and 'bad' molecules-it just reacts to novelty. Apixaban isn't toxic; it's just unfamiliar enough to trigger a misfire. That's why reactions can appear months later. It's not a flaw in the drug-it's a flaw in our biological recognition system. We're still learning how to predict these things.
Alyssa Salazar
November 8, 2025 at 15:07Okay, but let’s be real-this is a pharmacovigilance nightmare. The 2.4% rate? That’s not negligible. And the fact that docs don’t screen for prior drug rashes? That’s just lazy. If you’ve had a reaction to any DOAC, you’re basically playing Russian roulette with your skin. We need mandatory baseline immunological profiling before prescribing. No more guesswork.
Beth Banham
November 9, 2025 at 06:09My mom had a rash on her legs after six months on apixaban. She was scared to say anything because she didn’t want to seem like she was complaining. This post made me realize how important it is to speak up-even if it feels small. She switched to edoxaban and it’s been perfect since.
Brierly Davis
November 10, 2025 at 19:32Just wanted to say-you’re not alone. I had the same thing. Itchy patches, no fever, just annoying as hell. Took me 3 weeks to connect it to the pill. Once I switched to dabigatran? Vanished in 4 days. Don’t wait. Talk to your doc. You’ve got options. 💪
Amber O'Sullivan
November 11, 2025 at 10:46Been on apixaban 18 months no issues but my cousin got a rash and her doctor told her it was stress. She ended up in the ER with fever and swelling. Don't let them dismiss it. If your skin changes listen to it
Jim Oliver
November 12, 2025 at 04:55Of course you can’t just stop apixaban. Because apparently, strokes are less scary than itchy skin. Classic medical gaslighting. Meanwhile, 89% resolve after switching? That’s not a side effect-that’s a product defect.
William Priest
November 13, 2025 at 03:34Apixaban? More like apix-a-banana. I’ve seen 3 patients with this exact rash. All of them were over 70 and had renal issues. You think this is rare? It’s just underreported because doctors don’t connect the dots. Wake up. It’s not an allergy-it’s a delayed T-cell response. Learn your immunology.