What Exactly Is Arthritis?
Arthritis isn’t just one disease. It’s more than 100 different conditions that all attack your joints. Some make your knees creak. Others make your fingers swell up like sausages. Some creep in slowly over years. Others hit like a storm-fatigue, fever, and pain all at once.
The two biggest players? Osteoarthritis and rheumatoid arthritis. Together, they make up nearly 9 out of 10 arthritis cases. But they’re as different as a worn-out shoe and a fire alarm going off inside your body.
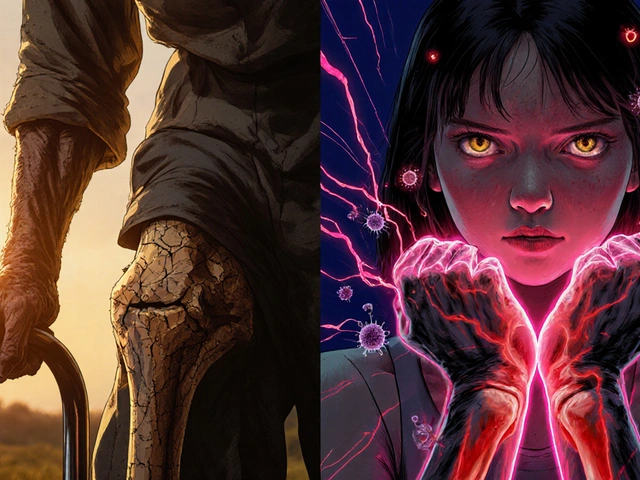
Osteoarthritis: The Wear and Tear Type
Osteoarthritis (OA) is what happens when the cushion between your bones-cartilage-wears down. Think of it like the rubber on your car tires. Over time, with use, it thins out. When that happens, bone starts grinding on bone. That’s when pain kicks in.
It usually shows up after 50, but not always. People who’ve had knee injuries, carried extra weight for years, or worked physically demanding jobs often get it earlier. It loves weight-bearing joints: knees, hips, lower back. But it’s also common in the hands-especially the joints at the very tips of your fingers and the middle knuckles.
Here’s what it feels like:
- Pain that gets worse when you move, better when you rest
- Morning stiffness that lasts less than 30 minutes
- A grating or crackling sound when you bend the joint
- Bony lumps (bone spurs) you can sometimes feel or see
Unlike other types, OA doesn’t make you tired. It doesn’t raise your temperature. It doesn’t attack your lungs or eyes. It stays in the joint. That’s why it’s called localized-it doesn’t spread through your body.
Rheumatoid Arthritis: The Body’s Betrayal
Rheumatoid arthritis (RA) is not about wear and tear. It’s about your immune system turning on you.
Your body has soldiers-white blood cells-that fight off germs. In RA, those soldiers get confused. They think your own joint lining (synovium) is an invader. So they attack it. That causes swelling, heat, and pain. Over time, this inflammation eats away at cartilage and bone. And it doesn’t stop at the joints.
RA can hit at any age-even in teens and young adults. It’s not rare in people under 40. And it doesn’t care which side of your body you’re on. It hits both sides at once. Both wrists. Both knees. Both ankles. Symmetry is its signature.
Here’s what RA feels like:
- Morning stiffness that lasts over an hour-sometimes all day
- Joints that feel hot, swollen, and tender to the touch
- Fatigue so deep it feels like you’ve run a marathon for a week
- Low-grade fevers, loss of appetite, weight loss
- Nodules-hard lumps under the skin, often near elbows
RA is a systemic disease. That means it can affect your heart, lungs, eyes, and even your blood vessels. Left untreated, it can destroy joints in months, not years.

How They’re Different: A Quick Side-by-Side
| Feature | Osteoarthritis (OA) | Rheumatoid Arthritis (RA) |
|---|---|---|
| Cause | Wear and tear on cartilage | Autoimmune attack on joint lining |
| Typical Age of Onset | Over 50 | Any age, including 20s-30s |
| Joint Pattern | Asymmetrical (one knee, not both) | Symmetrical (both hands, both knees) |
| Morning Stiffness | Less than 30 minutes | More than one hour |
| Systemic Symptoms | No fatigue, no fever | Fatigue, fever, weight loss, nodules |
| Commonly Affected Joints | Knees, hips, spine, DIP finger joints | MCP joints, wrists, PIP joints, ankles |
| Diagnosis | X-ray: joint space narrowing, bone spurs | Blood tests: RF, anti-CCP antibodies |
| Treatment Focus | Pain relief, weight loss, joint protection | Immune suppression, DMARDs, biologics |
Other Common Types of Arthritis
OA and RA aren’t the whole story. Two other types show up often enough to matter.
Gout: The Stone in Your Joint
Gout isn’t about aging or autoimmunity. It’s about uric acid. When your body makes too much-or can’t flush it out-it forms sharp crystals in your joints. The big toe? That’s ground zero. But ankles, knees, and fingers can get hit too.
It doesn’t creep in. It strikes like lightning: intense pain, redness, swelling, heat. One minute you’re fine. The next, you can’t put your sock on.
Triggers? Beer, red meat, sugary drinks, dehydration. It’s more common in men and people with kidney issues. Treatment? Medications to lower uric acid, plus lifestyle changes.
Psoriatic Arthritis: Skin and Joints Together
If you have psoriasis-those red, scaly patches on your skin-you’re at higher risk. Psoriatic arthritis can develop in up to 30% of people with psoriasis.
It often affects the fingers and toes, making them swell up like sausages (dactylitis). It can also cause lower back pain and nail changes-pitting, lifting, discoloration.
Like RA, it’s autoimmune. But it doesn’t always show up in blood tests. Diagnosis relies on symptoms, skin exams, and sometimes imaging.
Why Getting the Diagnosis Right Matters
Treating OA like RA? You’re giving someone powerful immune drugs for a problem that doesn’t need them. Side effects? Liver damage, infections, even cancer risk.
Treating RA like OA? That’s dangerous. If you wait to treat RA with just painkillers, you’re letting your immune system chew through your joints. Permanent damage can happen in as little as 3 to 6 months.
Doctors don’t just guess. They use tools:
- X-rays for OA: look for bone spurs and narrowing joint space
- Blood tests for RA: check for rheumatoid factor (RF) and anti-CCP antibodies
- Ultrasound for early RA: can spot inflammation before it shows on X-rays
- Physical exam: symmetry, swelling pattern, skin changes, nodules
And timing? It’s everything. For RA, starting DMARDs like methotrexate within the first few months can stop joint damage before it starts. For OA, losing just 5 kilograms can cut knee pain by half.

What You Can Do Today
If you’re dealing with joint pain, don’t wait. Don’t assume it’s just "getting older."
For OA:
- Move-even if it hurts a little. Walking, swimming, cycling protect your joints better than rest
- Manage your weight. Every extra pound adds 4 pounds of pressure on your knees
- Try physical therapy. Strengthening muscles around the joint takes stress off it
- Use heat or ice. Heat loosens stiff joints. Ice calms swelling
For RA:
- See a rheumatologist ASAP. Don’t wait for your GP to say "take an NSAID and come back."
- Stop smoking. It makes RA worse and reduces the chance of remission
- Follow your medication plan. DMARDs don’t work overnight. They need time
- Track your symptoms. Note which joints hurt, how long stiffness lasts, energy levels
Either way, don’t ignore fatigue, fever, or swelling that doesn’t go away. These aren’t normal signs of aging. They’re signals.
What’s New in Arthritis Care
Science is moving fast. In 2023, platelet-rich plasma (PRP) injections became more common for OA-though evidence is still mixed. For RA, new JAK inhibitors like tofacitinib give options when traditional drugs fail.
Researchers are now looking for blood markers that show cartilage breaking down before X-rays catch it. That could mean catching OA earlier than ever.
And for RA? Remission isn’t a dream anymore. With early, aggressive treatment, 30 to 50% of patients reach a point where symptoms vanish and joint damage stops.
Final Thought: Pain Isn’t Normal
Just because your knees crack doesn’t mean you have to live with pain. Just because your fingers swell doesn’t mean it’s "just arthritis."
Knowing the difference between osteoarthritis and rheumatoid arthritis isn’t just academic. It’s life-changing. One is managed. The other is controlled. One slows down. The other can stop.
Don’t let confusion cost you your mobility. Get tested. Know what you’re dealing with. And take action-before the damage becomes permanent.
Can you have both osteoarthritis and rheumatoid arthritis at the same time?
Yes. It’s not rare. Someone with RA can develop OA in the same joint from years of inflammation and wear. Or someone with OA from aging might later develop RA due to genetic or environmental triggers. Doctors look for overlapping symptoms and use blood tests and imaging to untangle them.
Does weather affect arthritis pain?
Many people report more pain during cold, damp weather. While no study proves weather causes arthritis, changes in barometric pressure may affect swelling and nerve sensitivity in already inflamed or damaged joints. It’s not the cause, but it can make symptoms feel worse.
Is arthritis hereditary?
OA has a weak genetic link-your risk increases if your parents had it, especially in the hands. RA has a stronger genetic component. If you carry the HLA-DRB1 gene, your risk is higher, especially if you smoke. But genes aren’t destiny. Lifestyle plays a huge role.
Can children get rheumatoid arthritis?
Children don’t get "rheumatoid arthritis"-they get Juvenile Idiopathic Arthritis (JIA). It’s similar in mechanism but has different subtypes and treatment approaches. JIA can start as early as age 1 and affects about 1 in 1,000 children. Early treatment is critical to prevent growth problems and joint damage.
Are there natural remedies that work for arthritis?
Some help with symptoms, but none cure the disease. Omega-3s from fish oil can reduce inflammation in RA. Turmeric has mild anti-inflammatory effects. Weight loss, exercise, and quitting smoking are the most powerful natural tools. But don’t replace prescribed meds with supplements-especially with RA. Delaying treatment can cause irreversible damage.




Jennifer Walton
November 15, 2025 at 18:14I used to think arthritis was just old people creaking. Turns out, it’s more like your body having an existential crisis. Some joints just give up. Others revolt. Either way, we’re all just bags of meat with bad software updates.
Still, I’m glad someone broke it down without jargon. I actually understand now.
Kihya Beitz
November 15, 2025 at 23:35Wow. Another article that makes me feel guilty for not being a rheumatologist. Next they’ll tell me to stop eating bread and start meditating on my synovial fluid.
Andrew Eppich
November 17, 2025 at 06:43It is deeply concerning that public health education remains so fragmented. The conflation of degenerative joint disease with systemic autoimmune pathology is not merely inaccurate-it is dangerous. Misdiagnosis leads to inappropriate pharmacological intervention, which in turn precipitates iatrogenic harm. This article, while lucid, underscores a broader societal failure in medical literacy.
Jessica Chambers
November 18, 2025 at 16:06I had no idea RA could hit you in your 20s 😳 My cousin thought she was just "stressed" for 8 months before getting diagnosed. Don't wait. Seriously.
Shyamal Spadoni
November 20, 2025 at 05:50You know what they dont tell you? The real cause of RA is 5G towers and glyphosate in the water. The government and Big Pharma dont want you to know that your immune system is being hacked by chemtrails and microchips in your coffee. I saw a guy on YouTube who cured his arthritis by drinking distilled water and sleeping with magnets under his pillow. He’s now running a retreat in Belize. The doctors? They’re all in on it. Why do you think they call it "autoimmune"? So you think it’s YOUR fault. But it’s not. It’s the system.
Katie Baker
November 20, 2025 at 10:21This literally saved my sanity. I’ve been Googling "why do my knuckles look like sausages" for weeks. Now I know it’s not just me being dramatic. 💪
John Foster
November 22, 2025 at 03:12There is a profound metaphysical truth in the distinction between osteoarthritis and rheumatoid arthritis. OA is the body’s quiet resignation to entropy. RA is the soul’s rebellion against its own vessel. We are not merely mechanical beings subject to wear. We are living systems, and when the immune system turns inward, it is not malfunctioning-it is screaming. Most people hear the noise but never listen. They mask it with NSAIDs and call it progress. But pain is not an error. It is a message. And we have forgotten how to decode it.
Perhaps the real cure is not in biologics, but in stillness. In listening. In surrender.
Edward Ward
November 23, 2025 at 01:44I appreciate the clarity here-especially the side-by-side table. But I’d like to add one thing: the overlap between psoriatic arthritis and RA is often underdiagnosed. I’ve seen patients with negative RF and anti-CCP, but clear nail pitting and dactylitis. Ultrasound is critical in these cases. Also, the myth that "weather doesn’t affect arthritis" needs to be retired-multiple biomechanical studies show barometric pressure shifts alter joint capsule pressure in inflamed tissues. It’s not placebo; it’s physics. And yes, I’ve tracked my own symptoms for 12 years. The correlation is real. Finally, thank you for mentioning that OA and RA can coexist. That’s a key point clinicians miss. It’s not either/or-it’s both/and. And that changes everything.