Crohn's disease and ulcerative colitis are both forms of inflammatory bowel disease, but they differ in location, depth of inflammation, complications, and treatment. Understanding these differences is key to proper diagnosis and care.
Inflammatory Bowel Disease: Causes, Treatments, and What You Need to Know
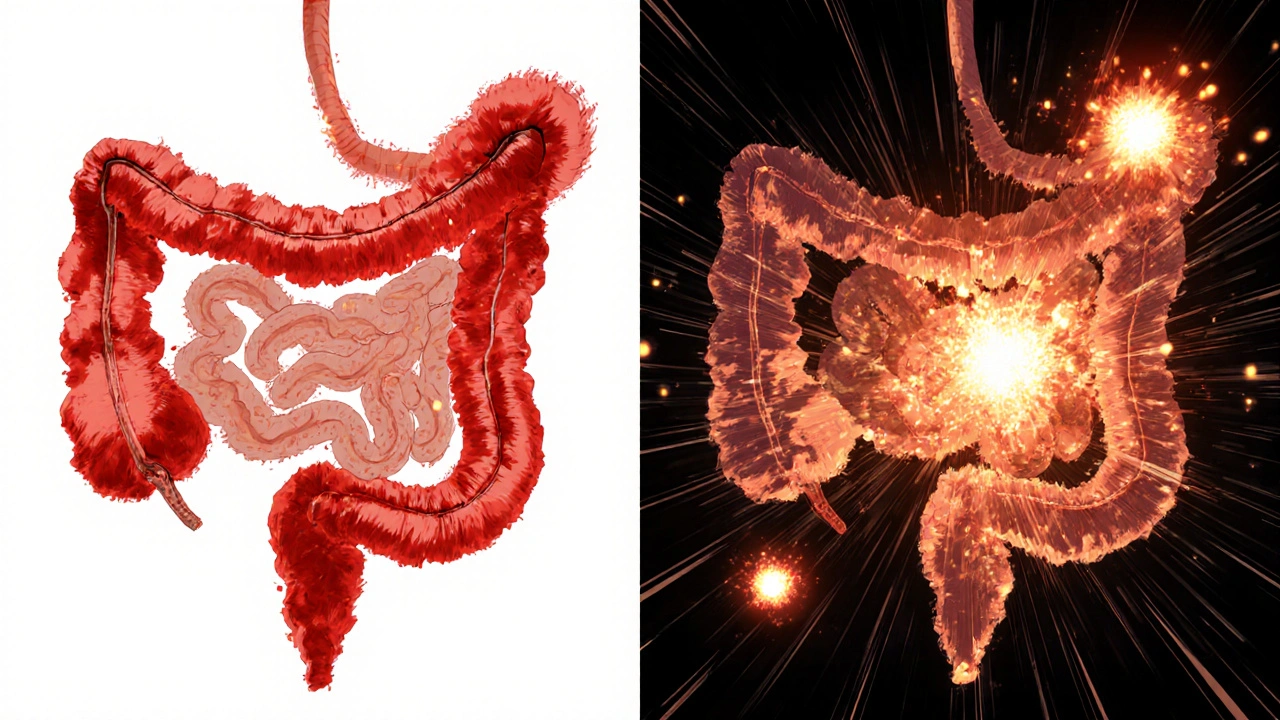
When you hear inflammatory bowel disease, a group of chronic conditions causing long-term inflammation in the digestive tract. Also known as IBD, it’s not the same as irritable bowel syndrome—IBD involves real tissue damage, not just spasms or sensitivity. Two main types drive most cases: Crohn's disease, can affect any part of the GI tract from mouth to anus, often skipping areas and digging deep into tissue layers, and ulcerative colitis, limited to the colon and rectum, causing continuous ulcers and surface inflammation. Both are autoimmune in nature, meaning your immune system mistakenly attacks your own gut lining, leading to pain, diarrhea, weight loss, and fatigue.
What triggers IBD isn’t fully understood, but genetics, gut bacteria imbalances, and environmental factors like smoking or processed diets play big roles. Unlike occasional stomach upset, IBD doesn’t go away with a change in food or stress relief—it needs medical management. Treatments range from anti-inflammatory drugs like aminosalicylates to biologics that target specific immune signals, and sometimes surgery if damage is severe. Many people also use supplements like probiotics or vitamin D to support gut healing, though these don’t replace prescribed meds. The goal isn’t just to silence symptoms but to put the disease into remission and prevent long-term complications like strictures or colon cancer.
People with IBD often juggle multiple meds, frequent doctor visits, and lifestyle tweaks to stay stable. That’s why understanding your options matters—whether it’s choosing between oral pills or injectables, knowing when to escalate therapy, or spotting early signs of a flare before it hits hard. The posts here give you real, no-fluff info on how these treatments work, what side effects to watch for, and how to talk to your doctor about switching or adding meds. You’ll also find guidance on managing IBD alongside other conditions like arthritis or skin issues that sometimes come with it. This isn’t theory—it’s what people living with IBD actually need to know to take control.