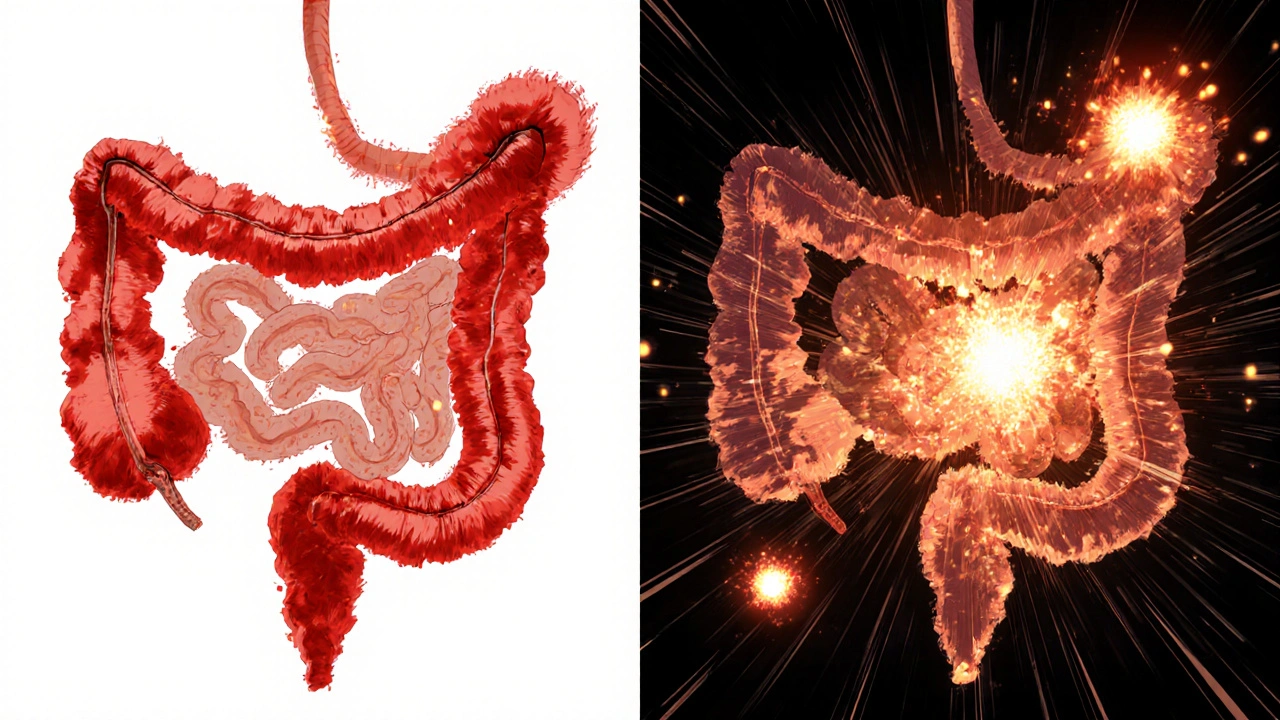
Crohn's disease and ulcerative colitis are both forms of inflammatory bowel disease, but they differ in location, depth of inflammation, complications, and treatment. Understanding these differences is key to proper diagnosis and care.
IBD: Understanding Inflammatory Bowel Disease and Treatment Options
When people talk about IBD, a group of chronic conditions that cause inflammation in the digestive tract. Also known as inflammatory bowel disease, it’s not the same as irritable bowel syndrome—IBD involves real tissue damage, not just discomfort. The two main types are Crohn’s disease, a condition that can affect any part of the GI tract from mouth to anus and ulcerative colitis, limited to the colon and rectum, causing ulcers and constant inflammation. Both lead to ongoing symptoms like diarrhea, abdominal pain, weight loss, and fatigue. Unlike temporary gut issues, IBD doesn’t go away with a change in diet or stress management alone—it needs medical tracking and often long-term treatment.
What makes IBD tricky is how it connects to other parts of your health. Flares can be triggered by infections, antibiotics, or even smoking. Some people with IBD develop joint pain, skin rashes, or eye inflammation because the immune system attacks more than just the gut. Medications like biologics, immunomodulators, and aminosalicylates aim to calm that overactive immune response. But not all drugs work for everyone. What helps one person might do nothing for another, which is why finding the right treatment often feels like trial and error. And while surgery can remove damaged sections of the intestine, it’s not a cure—especially in Crohn’s, where inflammation can return elsewhere.
There’s growing evidence that gut health plays a bigger role than we once thought. Diet, microbiome balance, and even mental stress can influence how IBD behaves. Some people find relief with specific diets like low-FODMAP or exclusive enteral nutrition, while others rely on supplements like vitamin D or probiotics to support recovery. But none of these replace medical care. The key is working with a specialist who understands the full picture—not just the symptoms, but how IBD affects your life long-term. Below, you’ll find real-world guides on managing side effects, understanding drug interactions, and making sense of treatment choices that actually matter.