When a vertebra in your spine cracks under pressure - often from osteoporosis, a fall, or cancer - the pain can be unbearable. Standing, sitting, even breathing becomes a struggle. For years, the only options were weeks of bed rest, painkillers, or risky open surgery. Today, two minimally invasive procedures have changed the game: kyphoplasty and vertebroplasty. Both use medical-grade bone cement to stabilize broken spinal bones, but they’re not the same. Knowing the difference can mean faster relief, lower risk, and better long-term outcomes.
How These Procedures Work
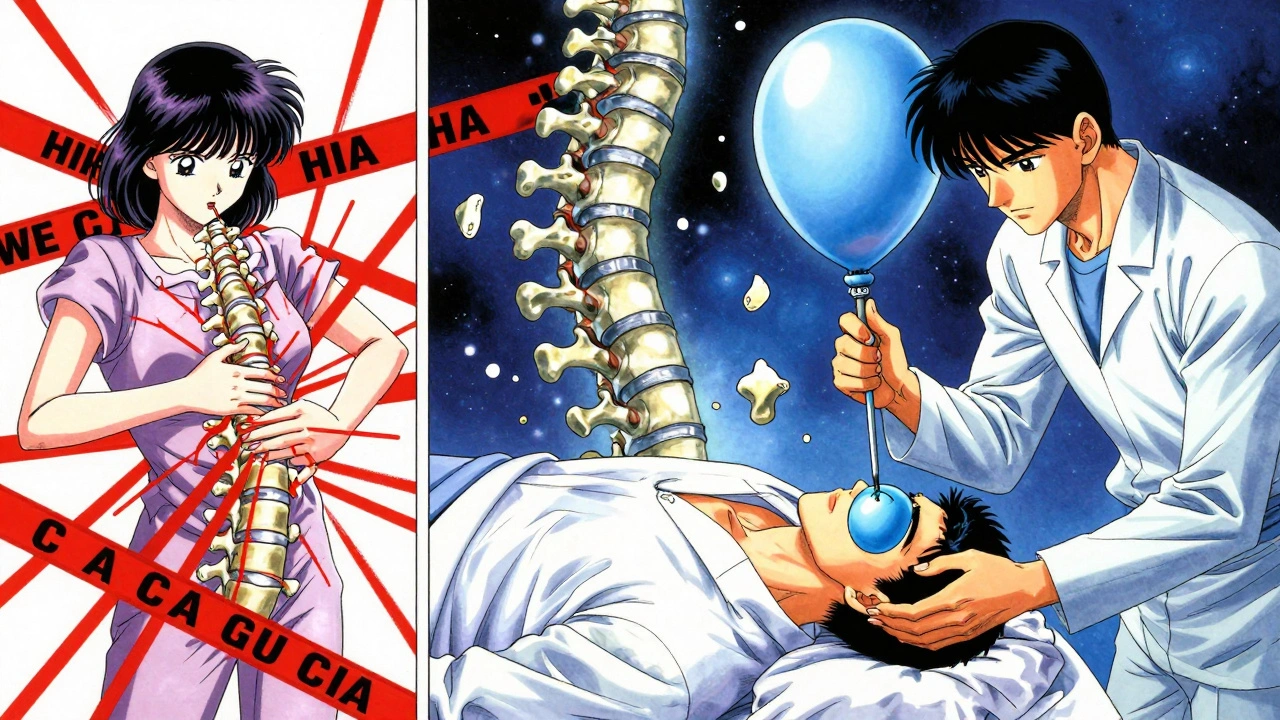
Both kyphoplasty and vertebroplasty are done through a tiny needle inserted through your back, guided by real-time X-ray imaging. You’re awake but sedated, and the whole thing takes about 30 to 60 minutes. The goal? Stop the pain and let you get back on your feet - often the same day.Vertebroplasty is the older method. Developed in France in the 1980s, it involves injecting liquid bone cement - polymethylmethacrylate, or PMMA - directly into the fractured vertebra. The cement hardens in 10 to 20 minutes, acting like an internal cast that holds the bone together. It’s simple, fast, and effective.
Kyphoplasty, developed in the late 1990s, adds a crucial step. Before injecting cement, a small balloon is inserted into the fractured bone and gently inflated. This creates a cavity and can lift the collapsed vertebra back toward its normal height. Once the balloon is deflated and removed, cement is injected into the space it left behind. The idea? Not just to stop the pain, but to fix the shape of the spine.
Which One Fixes Height Loss?
If your spine has started to curve forward - what doctors call kyphosis - kyphoplasty has a clear edge. Studies show it can restore 40% to 60% of the height lost in a compression fracture. Vertebroplasty? It barely moves the needle. The cement fills the crack but doesn’t lift the bone.But here’s the catch: that restored height doesn’t always last. A 2007 study in Spine found that after just 500 daily movements - like walking or standing - the vertebra loses about 30% of the height gained during kyphoplasty. So while the procedure looks better on an X-ray, the real-world benefit might be more about stability than posture.
Pain Relief: Is One Better?
When it comes to pain, both procedures deliver almost identical results. Research from Central Oregon Radiology shows 85% to 90% of patients report immediate pain relief after either procedure. Pre-procedure pain scores on the Visual Analog Scale (VAS) average 8.2 out of 10. Within 24 hours, that drops to 1.5. That’s not just improvement - it’s life-changing.Patients on forums like Reddit and SpineUniverse describe it like flipping a switch. One user wrote, “I went from 9/10 pain to 2/10 within hours.” Another, who had vertebroplasty, said, “The constant 7/10 pain became occasional 3/10.” Neither procedure guarantees 100% relief - about 10% to 15% of patients still feel some discomfort - but for most, it’s the fastest way out of severe pain.
Complications: Risk Comparison
Cement leakage is the biggest concern with both procedures. When cement escapes the bone and enters nearby tissue, it can press on nerves or even travel to the lungs. Vertebroplasty has a much higher leak rate - anywhere from 27% to 68% of cases. Kyphoplasty cuts that risk in half, with leakage rates between 9% and 33%.Why? Because the balloon in kyphoplasty creates a controlled space for the cement to fill. In vertebroplasty, the cement is injected under high pressure (150-200 psi) into a fractured, porous bone - it can squirt out anywhere. Symptomatic leaks - the kind that cause real problems - happen in about 1.1% of vertebroplasty cases and 0.6% of kyphoplasty cases, according to a 2016 meta-analysis in The Spine Journal.
Another risk: new fractures in nearby vertebrae. About 5% to 10% of patients develop a new fracture within a year. This isn’t caused by the procedure itself, but by the fact that osteoporosis is still active. One broken bone often means others are weak too.
Cost and Accessibility
Kyphoplasty costs 20% to 30% more than vertebroplasty. In 2023, Medicare paid an average of $3,850 for kyphoplasty versus $2,950 for vertebroplasty. That’s because kyphoplasty uses a balloon system - a specialized device made by companies like Medtronic, Stryker, and DePuy Synthes, which control 85% of the market.But cost isn’t just about the procedure. Hospital stays, follow-ups, and rehab add up. Since both procedures let patients go home the same day and return to normal activities within 72 hours, the total recovery cost is far lower than open spinal fusion, which can require weeks of rehab and lost wages.
Medicare approves both procedures in over 95% of cases - as long as you’ve tried conservative treatments first. That means at least 4 to 6 weeks of pain medication, physical therapy, or a back brace with no improvement.
Who Gets Which Procedure?
There’s no one-size-fits-all answer. Your doctor will choose based on your fracture’s shape, age, and your overall health.- Choose kyphoplasty if: Your fracture is recent (within 6 weeks), the bone has collapsed more than 30%, you have visible spinal curvature, or you’re concerned about cement leakage risk.
- Choose vertebroplasty if: The fracture is stable, the bone hasn’t collapsed much, you’re on a tighter budget, or you’re older and less active.
Dr. Richard Jensen from Oregon Health & Science University argues that for simple fractures without deformity, vertebroplasty offers the same pain relief at a lower cost - making it the smarter choice for healthcare systems. Dr. John Kallmes, one of kyphoplasty’s inventors, agrees that both work well for pain, but says the height restoration benefit is often overhyped.

What Happens After the Procedure?
You’ll spend 4 to 6 hours recovering under observation. Most people walk within a few hours. You’ll be told to avoid heavy lifting or twisting for 24 hours. Normal activities - walking, light chores - can resume in a few days. Most patients stop using opioids within a week.Physical therapy is often recommended to strengthen core muscles and improve posture. But the real long-term work is treating the root cause: osteoporosis. Without it, you’re at risk for more fractures. Doctors will likely prescribe calcium, vitamin D, bisphosphonates, or other bone-strengthening drugs.
What’s New in 2025?
The field is evolving. New cement types - like calcium phosphate - are being used because they’re more like natural bone, produce less heat during hardening, and may bond better with your spine. Medtronic’s updated balloon system, approved in March 2023, allows more precise inflation and reduces procedure time.A major 2023 study in The Lancet found that patients who got either procedure within two weeks of their fracture had a 28% lower risk of dying within a year compared to those who only got pain meds. That’s huge. It suggests these aren’t just pain relievers - they might be life-savers.
Right now, a trial called COAST is tracking patients for two years to see if kyphoplasty’s height restoration leads to better mobility or less disability than vertebroplasty. Results are expected by late 2024. If kyphoplasty wins, its market share - already at 65% - could climb to 75% by 2028.
Real Patients, Real Outcomes
On Healthgrades, kyphoplasty has a 4.6/5 rating from over 1,200 reviews. Vertebroplasty sits at 4.4/5 from 800+ reviews. The top comments? “I was in a wheelchair. Now I’m gardening.” “No more morphine. No more fear of falling.” “I didn’t know life could feel this normal again.”But not everyone gets relief. Some still have pain. A few develop new fractures. That’s why these procedures aren’t magic - they’re tools. They fix broken bones, but they don’t fix osteoporosis.
If you’re considering one of these procedures, ask your doctor: Is my fracture recent? Is there height loss? What’s my risk of cement leakage? What’s the plan for my bones after this? The right answer isn’t always the most expensive one - it’s the one that matches your body, your life, and your goals.




David Brooks
December 7, 2025 at 00:08OMG I had kyphoplasty last year and I swear it was like someone flipped a switch in my spine. I was in a wheelchair, now I’m gardening at 7am with my grandkids. No more morphine, no more fear of falling. Life didn’t just get better-it got back. 🙌
Sadie Nastor
December 7, 2025 at 09:36i just got vertebroplasty last week and honestly? i’m still kinda in shock. the pain just… vanished. like, one minute i could barely breathe, next minute i was texting my sister from the recovery room. not perfect, but wow. 🤯
Nicholas Heer
December 8, 2025 at 07:30They’re lying about the balloon thing. You think they’re fixing your spine? Nah. It’s Big Pharma’s latest cash grab. The cement’s toxic, the balloon’s just a fancy way to charge you $9k, and they don’t tell you that 3 outta 5 patients end up with new fractures because the rest of your bones are rotting from glyphosate in the water supply. Wake up, sheeple.
Stacy here
December 9, 2025 at 03:15Let’s be real-this whole debate is a distraction. We’re treating symptoms while the system lets people age into osteoporosis because Medicare won’t cover preventative nutrition programs. Kyphoplasty? Cool. But why are we letting 70-year-olds live in food deserts with zero access to calcium-rich meals? The real fix isn’t in the OR-it’s in policy. And no, a vitamin D pill won’t fix capitalism.
Kyle Flores
December 9, 2025 at 21:57Hey everyone-just wanted to say I’m really glad so many of you are sharing your stories. I had vertebroplasty after a fall and honestly, I was terrified. But reading these posts? It helped me feel less alone. If you’re still healing, you’re doing better than you think. Take it slow. Walk a little each day. And don’t let anyone make you feel guilty for needing help. You’re not broken-you’re healing.
Olivia Hand
December 10, 2025 at 05:40Anyone else notice how the ‘height restoration’ claim feels like marketing fluff? Like, yeah, the X-ray looks pretty, but if you’re still hobbling after 6 months, does it matter? I’m more impressed by the 85% pain relief stat than the 40% height gain. The spine isn’t a Lego tower-it’s a living structure. Maybe we’re over-engineering the fix.
Louis Llaine
December 11, 2025 at 01:10So let me get this straight. You pay $3,850 to have a balloon inflated in your spine… just so you can go back to doing the same thing that broke it? Genius. I’m just waiting for the next ad: ‘Kyphoplasty Plus™ - now with Bluetooth pain tracking!’
Nancy Carlsen
December 11, 2025 at 14:39My mom had kyphoplasty and now she’s dancing at her friend’s wedding. 🕺💃 I cried watching her. It’s not just about pain-it’s about getting your joy back. If you’re scared, talk to someone who’s been there. You’re not alone. And yes, the cost sucks… but so does living in constant pain. 💛
Ted Rosenwasser
December 11, 2025 at 20:24For the record, kyphoplasty uses PMMA with a balloon catheter system designed for controlled cement delivery under fluoroscopic guidance-unlike vertebroplasty’s high-pressure, unguided infiltration. The 2023 Lancet study showed a 28% mortality reduction in early intervention cohorts. If you’re not citing peer-reviewed meta-analyses, you’re just noise. Also, stop using emojis. It’s unprofessional.