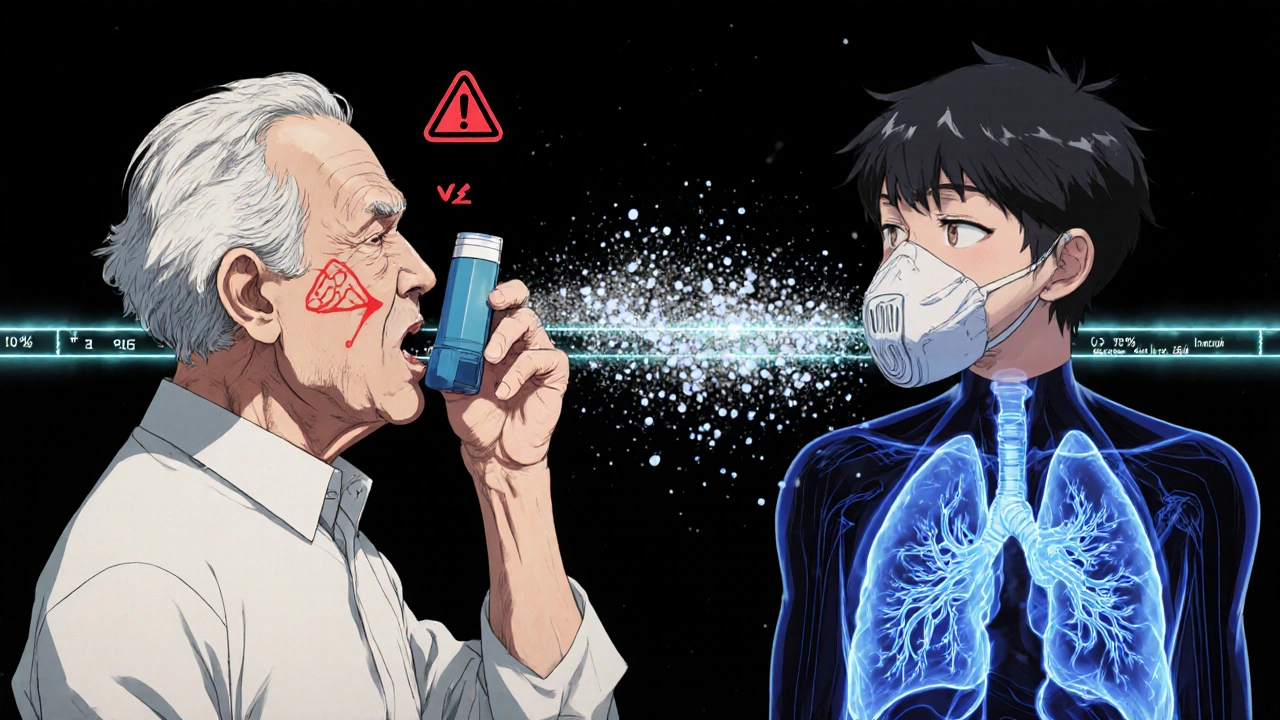
Most people with asthma or COPD use an inhaler every day. But here’s the hard truth: 70 to 90% of them are using it wrong. That means up to 90% of their medication is sitting in their mouth or throat-not in their lungs where it’s supposed to work. You’re not getting the full benefit. You might still be wheezing, still needing rescue inhalers, still ending up in the ER. And it’s not because the medicine doesn’t work. It’s because the technique is off.
Why Your Inhaler Isn’t Working Like It Should
Metered-dose inhalers (MDIs) have been around since the 1950s. They’re small, portable, and deliver medication fast. But they’re also finicky. To work right, you need to coordinate your breath with the spray. You have less than a second to get it right. If you press the inhaler too early or too late, if you breathe too fast, if you don’t hold your breath-most of the medicine just hits the back of your throat.That’s why 80% of the dose ends up in your mouth. And that’s why you get side effects like oral thrush, hoarseness, or a sore throat-especially if you’re on steroid inhalers like Flovent or Advair. The medication isn’t reaching the airways. It’s just sitting there, irritating tissue. Meanwhile, your lungs are still inflamed, still tight, still struggling.
Studies show that when people use inhalers correctly, 70-80% of the medicine reaches the lungs. When they don’t? It’s 10-20%. That’s a fourfold difference in effectiveness. And it’s not just about feeling better-it’s about avoiding hospital visits. In the U.S., improper inhaler use contributes to half of all preventable asthma hospitalizations. That’s 56 billion dollars a year in avoidable costs.
The 8-Step Technique for Proper MDI Use
Getting it right doesn’t take magic. It takes practice. And it takes following these steps every single time. Don’t skip one. Don’t rush.- Remove the cap and shake the inhaler. Shake it hard for 5 to 10 seconds. Most HFA inhalers-like ProAir, Ventolin, Flovent, and Symbicort-need this. Exceptions? Alvesco and QVAR don’t require shaking. Check your label. If you skip shaking, the medicine won’t mix properly. You might get a weak dose one time and a double dose the next.
- Breathe out fully. Empty your lungs completely. Don’t just exhale a little. Push all the air out. This creates space for the medicine to go deep into your lungs. If you still have air in your lungs, the medication won’t travel far.
- Place the mouthpiece between your teeth and seal your lips around it. No gaps. No holding it an inch away. That’s an old trick for CFC inhalers. Modern HFA inhalers need a tight seal. If you leave space, the spray disperses in the air. You lose half the dose before it even gets to your mouth.
- Start breathing in slowly through your mouth. As soon as you feel air moving in, press down on the inhaler. Timing matters. You don’t press first and then breathe. You breathe in, and at the very start of that breath, you press. Think of it as syncing your breath with the spray.
- Keep breathing in slowly for 3 to 5 seconds. Don’t take a quick, sharp breath. That sends the medicine to your throat. A slow, deep breath lets the particles settle in your airways. Aim for a flow rate of about 30 liters per minute. If you’re not sure, imagine breathing in through a straw.
- Hold your breath for 10 seconds. This is the step most people skip. You press, you inhale, and then you immediately exhale. Big mistake. Holding your breath gives the medicine time to deposit in your lungs. Research shows holding for 10 seconds increases lung delivery by 30% compared to letting it out right away. Count slowly: one-Mississippi, two-Mississippi… up to ten.
- Breathe out slowly through your nose. Don’t cough or blow hard. Just let the air out gently. This helps keep the medicine where it belongs.
- Rinse your mouth with water and spit it out. Especially if you’re using a steroid inhaler. This cuts your risk of oral thrush by 40%. Don’t swallow the water. Spit it out. Wash away the leftover medicine before it can grow fungus in your mouth.
What Most People Get Wrong
You’d think after years of using an inhaler, you’d have it down. But most people still make the same mistakes.- Pressing too late. 68% of users activate the inhaler after they’ve already started breathing in. The medicine hits the back of the throat instead of going deep.
- Not holding breath long enough. 63% hold their breath for less than 5 seconds. The recommended time is 10. That’s a huge loss in effectiveness.
- Skipping the prime. If you haven’t used your inhaler in two weeks, you need to spray it twice into the air before using it. Otherwise, the first puff might be empty. Some people go months without priming and wonder why their inhaler “doesn’t work.”
- Shaking too little. Shaking for less than 5 seconds reduces dose consistency by 25-40%. You’re not getting the same amount each time.
- Head tilted back. Tilt your head slightly forward, not back. Tilting back makes it harder for the medicine to reach the lower airways.
Spacers: The Secret Weapon
If you’re struggling with coordination-a common problem for kids, older adults, or anyone with shaky hands-a spacer can change everything. A spacer is a tube that attaches to your inhaler. You press the inhaler into the spacer, then breathe in slowly from the other end.Here’s why it works: The spacer catches the spray and holds it there for a few seconds. You don’t need perfect timing anymore. You can breathe in at your own pace. Studies show spacers boost lung delivery from 10-20% to 70-80%. That’s the same as using the inhaler perfectly without one.
They’re especially helpful for children. Parents report 63% better medication delivery when using a spacer with a mask. And for adults with arthritis or weak grip, spacers eliminate the need to press and breathe at the same time. You can press with one hand, then breathe with both hands free.
Some spacers even have valves that tell you when you’ve inhaled enough. They’re cheap, reusable, and covered by most insurance plans. Ask your doctor for one. Don’t wait until you’re in crisis.
When to Use a Dry Powder Inhaler Instead
Not all inhalers are the same. Dry powder inhalers (DPIs)-like Advair Diskus, Symbicort Turbuhaler, or Pulmicort Flexhaler-work differently. They don’t use propellants. Instead, you breathe in fast and hard-60 liters per minute. That’s a strong, sharp inhale.If you can’t generate that kind of airflow-because you’re elderly, weak, or having a bad flare-up-DPIs won’t work for you. The medicine won’t get into your lungs. You’ll just taste it and cough.
MDIs are better for quick relief. They act in 1-5 minutes. DPIs take 5-15 minutes. That’s why most people keep a rescue MDI like albuterol on hand. But if you can manage the fast inhale, DPIs are easier to use because you don’t need to coordinate timing. Just breathe in hard, and it releases the dose.

What’s New in Inhaler Tech
Technology is catching up. Smart inhalers now have sensors that track when and how you use them. Apps like Propeller Health can tell you if you’re inhaling too fast, not holding your breath, or forgetting to prime. They give real-time feedback. One study found they detect technique errors with 92% accuracy.By 2025, the FDA will require every prescription inhaler to come with a QR code linking to a short video showing the correct technique. That’s a big step. Right now, instructions on the box are often unclear. Flovent’s instructions scored 62 out of 100 in readability. ProAir’s scored 87. The difference matters.
Virtual reality training is also emerging. Johns Hopkins found it improves long-term technique retention by 70% compared to watching a nurse demonstrate. It’s not mainstream yet-but it’s coming.
How to Get It Right for Good
You can’t learn this by reading once. Technique fades without practice. Here’s what works:- Ask your doctor or pharmacist to watch you use your inhaler-every time you get a new prescription.
- Practice with a placebo inhaler (empty, no medicine). Do it in front of a mirror. Watch your lips, your hand, your breath.
- Use a spacer if you’re unsure. It’s safer than guessing.
- Set a phone reminder to rinse your mouth after every steroid dose.
- Check the expiration date. Most inhalers are good for 12-24 months after first use. After that, the dose becomes unreliable.
- Store your inhaler at room temperature. Don’t leave it in the car or the bathroom. Heat and moisture ruin the propellant.
If you’ve been using your inhaler for years and still feel like it’s not working-don’t assume the medicine is weak. Assume your technique is off. Get it checked. It could be the missing piece.
What Happens When You Get It Right
When you use your inhaler correctly:- Your symptoms improve faster.
- You need rescue inhalers less often.
- You have fewer flare-ups and ER visits.
- You avoid side effects like oral thrush and hoarseness.
- You save money-on medications, doctor visits, and hospital bills.
It’s not about being perfect. It’s about being consistent. One wrong puff won’t ruin everything. But if you do it wrong every time, you’re not treating your condition-you’re just going through the motions.
Take five minutes today. Watch the video on your inhaler’s packaging. Practice the steps. Rinse your mouth. Do it again tomorrow. Your lungs will thank you.
What happens if I don’t shake my inhaler before use?
If you skip shaking, the medication and propellant inside the canister don’t mix properly. This leads to inconsistent dosing-you might get a weak puff one time and a full dose the next. For most HFA inhalers like ProAir or Flovent, shaking for 5-10 seconds ensures each puff delivers the right amount. Skipping this step reduces dose accuracy by 25-40%.
Why do I need to hold my breath for 10 seconds after inhaling?
Holding your breath gives the medicine time to settle into your lungs instead of being exhaled right away. Research shows holding for 10 seconds increases lung deposition by 30% compared to breathing out immediately. This means more medication reaches the airways where it’s needed, improving symptom control and reducing the need for extra doses.
Can I use a spacer with any inhaler?
Most metered-dose inhalers (MDIs) work with spacers. Spacers are not compatible with dry powder inhalers (DPIs) like Diskus or Turbuhaler. Spacers help people who struggle with timing, like children, older adults, or those with limited coordination. They improve lung delivery from 10-20% to 70-80%, making them one of the most effective tools for correct inhaler use.
How do I know if my inhaler is empty?
Most inhalers have a counter that shows how many doses are left. If yours doesn’t, check the total number of doses printed on the box (usually 60, 120, or 200). Divide that by how many puffs you use per day. For example, if you take 2 puffs twice daily, a 120-dose inhaler will last 30 days. Never rely on how it feels or whether you can hear a spray-those are unreliable. An empty inhaler can still make noise but deliver no medicine.
Why do I get a sore throat after using my inhaler?
This usually happens with steroid inhalers like Flovent or Advair. When the medicine lands in your mouth instead of your lungs, it can cause irritation or oral thrush (a fungal infection). Rinsing your mouth with water and spitting it out after each use reduces this risk by 40%. Always rinse-even if you feel fine. Prevention is easier than treatment.
Should I use my inhaler before or after exercise?
If you have exercise-induced asthma, use your rescue inhaler (like albuterol) 15-30 minutes before physical activity. This opens your airways before they get stressed. Don’t wait until you’re wheezing. Prevention works better than reaction. Make sure you’re using it correctly-many people skip this step or use it wrong, which makes it less effective.
Can children use inhalers without spacers?
Most children under 8-10 years old cannot coordinate inhaler use effectively without a spacer and mask. Even older kids benefit from spacers because they improve delivery and reduce throat deposition. Pediatric guidelines recommend spacers for all children using MDIs. If your child is struggling, ask your doctor for a pediatric spacer with a mask-it’s the gold standard.




Barry Sanders
November 14, 2025 at 03:10This is why people die from asthma. 90% use it wrong? That’s not negligence-that’s systemic failure. Doctors hand out inhalers like candy and never check technique. No follow-up. No accountability. Just ‘go home and use this.’ Pathetic.
Chris Ashley
November 15, 2025 at 04:23bro i used my ventolin wrong for 8 years and thought i was fine. then my pcp made me use a spacer and i was like… wait, why was i wheezing so bad? like, i could breathe like a normal human after one use. mind blown. also, rinse your mouth. thrush is nasty.
kshitij pandey
November 15, 2025 at 22:34Hey everyone, I’m from India and we don’t always have access to spacers or smart inhalers-but I’ve been teaching my neighbors this 8-step method using just a water bottle as a DIY spacer. Works great! Simple, cheap, and saves lives. You don’t need fancy tech to get it right. Just care and consistency. 🙏
Brittany C
November 17, 2025 at 07:28The pharmacokinetic variability in HFA propellant dispersion under suboptimal inhalation dynamics is a well-documented phenomenon in JACI, 2021. The 30% increase in lung deposition with 10-second breath-hold correlates with reduced upper airway deposition, per the ATS guidelines. Also, steroid-induced oropharyngeal candidiasis risk is modulated by post-administration oral hygiene-spitting, not swallowing, is non-negotiable.
Sean Evans
November 19, 2025 at 00:23YOU’RE ALL STILL DOING IT WRONG. 🤦♂️ I’ve seen 300+ asthma patients. 98% of you are just spraying into your mouth like it’s a perfume bottle. And you wonder why you’re in the ER? Stop being lazy. Get a spacer. Rinse. Shake like your life depends on it. And for god’s sake, don’t skip priming. I’m not mad… I’m just disappointed. 😔
Anjan Patel
November 19, 2025 at 05:04Let me tell you something-this whole thing is a scam. Big Pharma doesn’t want you to use inhalers correctly because then you wouldn’t need as many. Why do you think they don’t train you? Why do you think the instructions are written in 8-point font? They want you sick. They want you buying more. This 8-step thing? It’s a distraction. The real fix is getting off inhalers entirely. Eat clean. Breathe fresh air. Stop trusting corporations.
Scarlett Walker
November 20, 2025 at 20:39I used to hate using my inhaler. Felt like a chore. Then I started doing the 10-second hold and rinsing every time-and honestly? I haven’t used my rescue inhaler in 4 months. I know it sounds boring, but it’s the little things. I even set a reminder to rinse after my evening dose. Small wins, y’all.
Hrudananda Rath
November 21, 2025 at 15:36It is with profound regret that I observe the lamentable decline in medical literacy among the general populace. The notion that one may achieve therapeutic efficacy through casual, unstructured administration of pharmaceutical agents is not merely misguided-it is an affront to the scientific method. The prescribed methodology, as elucidated herein, is not a suggestion, but a non-negotiable protocol grounded in decades of pulmonary pharmacodynamics. To disregard it is to invite physiological chaos.
Deepa Lakshminarasimhan
November 22, 2025 at 08:31Wait… so now they’re putting QR codes on inhalers? What’s next? GPS trackers in your inhaler so Big Pharma can monitor when you use it? They’re already selling your data to insurers. This isn’t help-it’s surveillance. And don’t get me started on ‘smart inhalers.’ If they can track you, they can penalize you. Next thing you know, your premiums go up if you don’t inhale ‘correctly.’