PAMORAs like methylnaltrexone, naloxegol, and naldemedine target opioid-induced constipation without affecting pain relief. Learn how they work, who benefits most, and what to expect from treatment.
Methylnaltrexone: What It Is, How It Works, and When It's Used
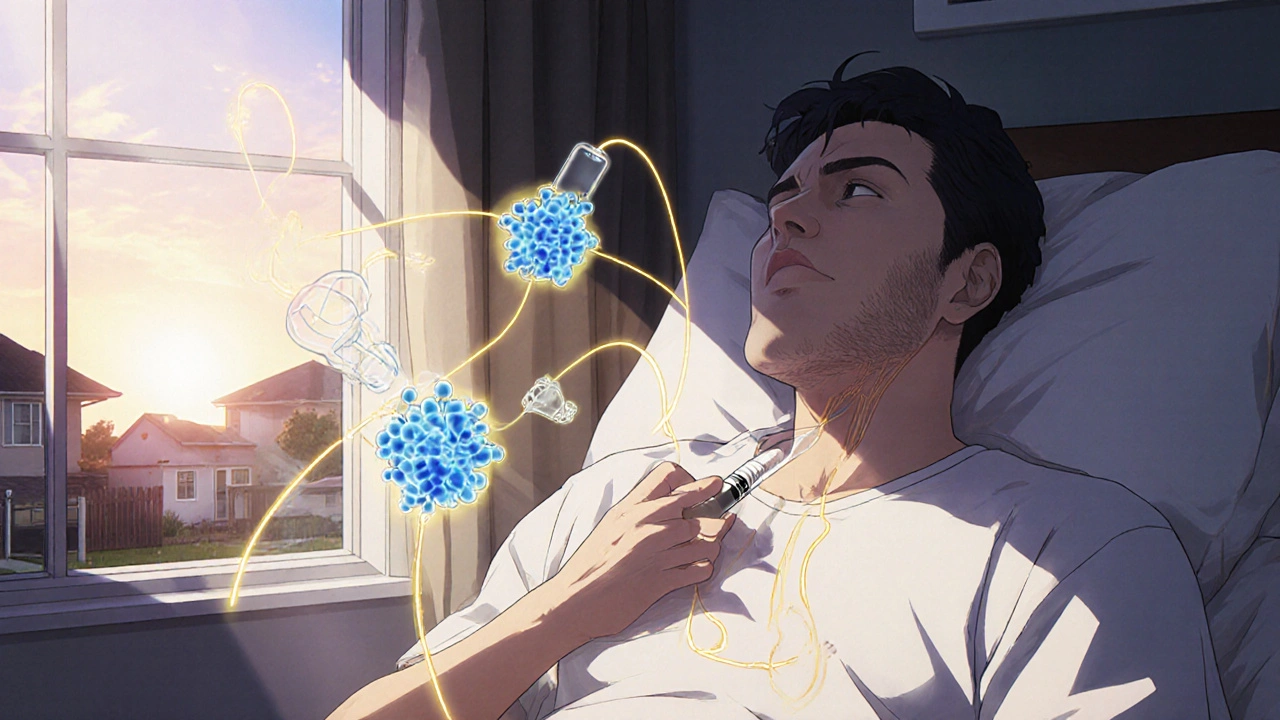
When you're taking strong pain meds like morphine or oxycodone, constipation often comes along as an unwanted side effect. That’s where methylnaltrexone, a peripherally acting mu-opioid receptor antagonist used to treat opioid-induced constipation without affecting pain control. Also known as Relistor, it works right in the gut, not the brain. Unlike regular laxatives, methylnaltrexone doesn’t just stimulate bowel movement—it blocks opioids from slowing down your digestive tract. That means you get relief without losing pain relief, which is why it’s often used in people on long-term opioids for cancer, chronic pain, or palliative care.
This drug isn’t for everyone. It’s meant for adults who’ve tried other laxatives and still can’t go. It’s not a first-line fix. Doctors usually reach for it when constipation becomes severe enough to affect quality of life or lead to complications like bowel obstruction. You’ll typically get it as a subcutaneous injection, though there’s also an oral version for some cases. The key benefit? It works fast—often within 30 minutes to 4 hours. And because it doesn’t cross the blood-brain barrier, it won’t interfere with how your pain meds work. That’s a big deal for people who rely on those drugs to function.
Methylnaltrexone relates closely to other opioid antagonists like naloxone, but it’s designed differently. Naloxone reverses overdoses by acting everywhere, including the brain. Methylnaltrexone is built to stay outside the central nervous system, targeting only gut receptors. That’s why it’s safer for long-term use in chronic pain patients. It also connects to broader topics like palliative care, where managing side effects is as important as treating the illness. People in hospice or those with advanced disease often face a tough balance: enough pain control without losing dignity through constipation. Methylnaltrexone helps keep that balance.
It’s not a cure-all, though. Some people still need to combine it with stool softeners or fiber. And it’s not cheap—insurance often requires prior authorization, similar to how they handle other specialty meds. But for those who’ve struggled with opioid-induced constipation for months or years, this drug can be a game-changer. You’ll find posts here that dig into how it compares with other treatments, what side effects to watch for, and how it fits into larger medication safety conversations. Whether you’re a patient, caregiver, or provider, the articles below give you real, practical insights—not just theory.