EHR integration connects pharmacies and providers to improve prescription safety, reduce errors, and cut hospital readmissions. Learn how it works, why most pharmacies still lack it, and what’s changing in 2025.
Electronic Prescribing: How Digital Prescriptions Are Changing Healthcare
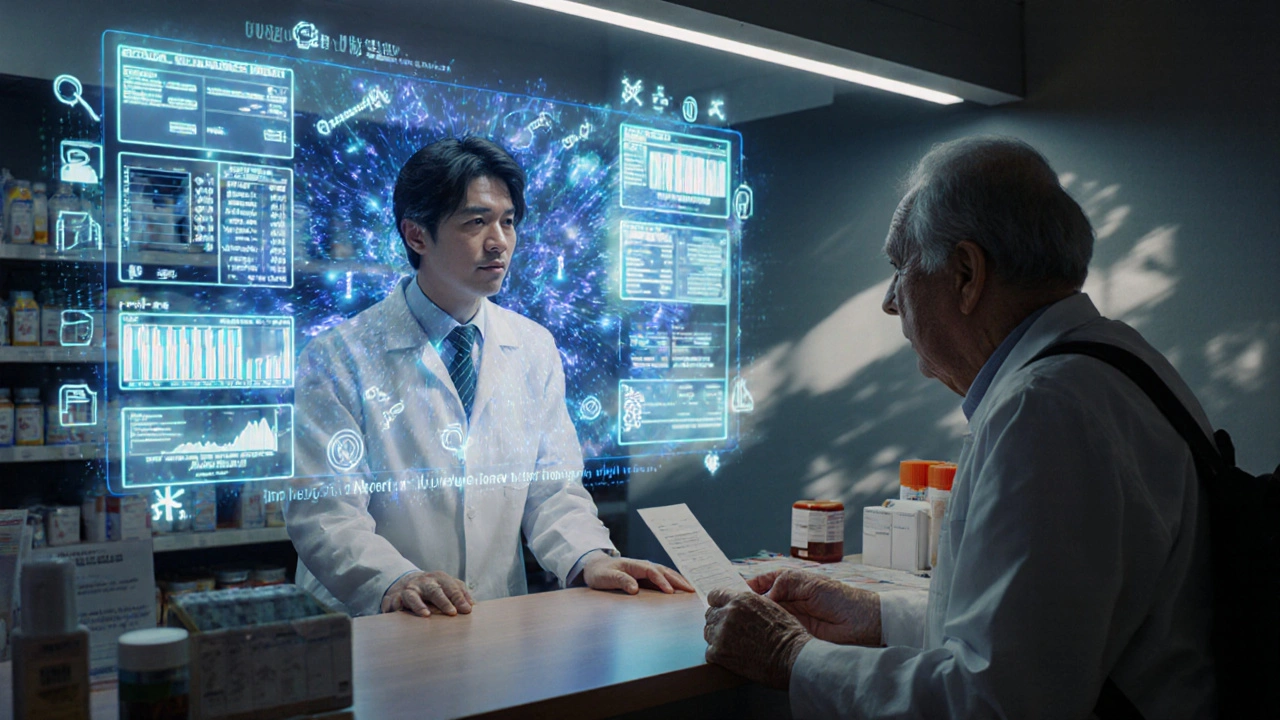
When a doctor sends your prescription straight to the pharmacy through a computer system, that’s electronic prescribing, a digital method of transmitting prescriptions from healthcare providers to pharmacies without paper or fax. Also known as e-prescribing, it’s one of the quietest but most powerful shifts in modern medicine. No more scribbled notes you can’t read. No more calls between pharmacies and clinics trying to figure out if a dose is 5 mg or 50 mg. This isn’t science fiction—it’s happening right now, in clinics and hospitals across the country.
Electronic prescribing isn’t just about replacing paper. It’s connected to e-prescribing systems, software platforms that integrate with electronic health records and check for drug interactions, allergies, and insurance coverage in real time. These systems flag dangerous combos before they’re even sent—like mixing blood thinners with certain antibiotics—or suggest cheaper generic alternatives. They also let pharmacists know instantly if a prescription was canceled or changed, reducing confusion and delays. And for patients? It means fewer trips back to the doctor’s office just to fix a typo, and faster pick-up times at the pharmacy.
Behind every smooth e-prescribe is a chain of people: doctors using tablets at the bedside, pharmacists verifying dosages on screens, and even insurers approving coverage before you walk in. It’s tied to digital health records, centralized systems that store your medical history, allergies, and past prescriptions so any provider can see what you’ve been taking. That’s why you might notice your new doctor already knows about the medication you’ve been on for years—even if you never told them. That’s the power of connected data.
But it’s not perfect. Some systems still don’t talk to each other. Rural clinics might still rely on fax machines. And not every pharmacy accepts every e-prescribe platform. Still, the trend is clear: paper prescriptions are fading fast. The data shows e-prescribing cuts medication errors by up to 50% and reduces unnecessary calls to doctors by nearly 30%. That’s not just convenience—it’s safety.
In this collection, you’ll find real, practical guides on how electronic prescribing works in daily practice. From how pharmacists handle substitutions under new rules, to how insurance denials get appealed when a digital script gets flagged, to how patients can track their own meds through digital portals. You’ll see how this tech connects to things like opioid safety, generic copays, and even how nurses and doctors are trained to use these systems in 2025. This isn’t about theory. It’s about what’s actually happening on the ground—and how it affects your health, your bills, and your time.